The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2005;58(03-04)
Content
[Application of the Multiple Sclerosis Functional Composite in Debrecen]
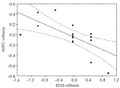
[Introduction - The Multiple Sclerosis Functional Composite (MSFC) has been recommended by the National Multiple Sclerosis Society as a new clinical outcome measure. It is based on measurements in three clinical dimensions: leg function/ambulation (timed 25-foot walk), arm function (9-hole peg test), and cognitive function (paced auditory serial addition test). Scores on component measures are converted to standard scores (Z-scores) that reflect patient performance. This method has not yet been introduced into routine clinical practice. Patients and method - MSFC calculation was applied to 17 patients with relapsing-remitting multiple sclerosis (age mean: 37.4±10.8 years; duration of the disease: 5.5±4.9 years, EDSS: 2.7±1.4) seen at the neuroimmunological outpatient clinic to evaluate its usefulness and its correlation with the traditionally applied Expanded Disability Status Scale (EDSS) and with patient-reported quality of life. Fifteen patients received immunomodulatory treatment (interferon beta and glatiramer acetate). MSFC and EDSS were measured at 0, 3, 6, 9, 12, 18 months, and questionnaires on quality of life were filled in by the patients at 0, 6, 12, 18 months of follow- up. Results - The prospective study confirmed a strong correlation between EDSS and MSFC (Spearman correlation test, p=0.03, 0.004, 0.002, 0.004, 0.0008, 0.002; R=-0.54, -0.66, -0.68, -0.65, -0.73, -0.69) in multiple sclerosis. The MSFC was more sensitive to clinical changes than EDSS. The extent of changes on the two scales correlated only after 18 months (p<0.005, R=-0.65). The arm/hand function was the most sensitive measure for disease progression. There was no correlation between the quality of life and either of the two other clinical parameters. Conclusion - MSFC is a simple method, suitable for followup of multiple sclerosis patients in everyday clinical practice.]
[Clinical neurosciences for efficient treatment - 2nd Live Issue of Clinical Neuroscience/ Ideggyógyászati Szemle]
[Clinical neurosciences for efficient treatment - 2nd Live Issue of Clinical Neuroscience/ Ideggyógyászati Szemle 2005;58(03-04)]
[CLINICO-PATHOLOGY AND DIFFERENTIAL DIAGNOSIS OF BINSWANGER’S DISEASE]
[Pathologically, Binswanger’s disease is subcortical periventricular leucoencephalopathy sparing the U fibers. Clinically it is characterised by executive dysfunction, gait problems, urinary incontinence, pseudobulbar palsy, mood disturbances and dementia. The pathomechanism of Binswanger’s disease is unclear. It is hypothesized that it results from an ischemic-hypoxic injury of the periventricular white matter, which, in turn, can be caused by a sclerotic elongation of the medullary arteries, widening of the perivascular spaces or decreased brain perfusion due to hypotension or heart disease. The symptoms of Binswanger’s disease frequently overlap with those of normal pressure hydrocephalus, vascular parkinsonism and Alzheimer’s disease. A diagnostic criterion of Binswanger’s disease is radiologically demonstrated leukoaraiosis, which, on the other hand, is not equivalent with Binswanger’s disease. A good clinical response after lumbar puncture or shunt implantation might lead to confusion with normal pressure hydrocephalus, which further complicates the clinical diagnosis. It is likely that among the above mentioned disorders there are a number of transitional forms and overlaps, which might be explained by the common pathomechanism of disturbance in cerebrospinal fluid circulation.]
[Supplementary sensory-motor seizures - symptomatology, etiology, and surgical management with illustrative case reports]
[In the past decade, owing to the advance of epilepsy surgery, growing knowledge has accumulated on the role of the supplementary motor area, described by Penfield and coworkers in the early fifties, in movement regulation and on the characteristics of seizures involving this area. In the Hungarian neurological literature this topic - despite its neurophysiological and practical clinical importance - has been hardly touched. The authors, based on their own experience obtained from surgeries performed within the framework of the "Co-operative Epilepsy Surgery Program", describe the electrophysiological features of this area, its role in movement regulation and the symptoms of epileptic seizures stemmed from or spread onto this area. Using cases as illustrations, they demonstrate the reasoning and various algorithms of the multidisciplinary examination necessary to explore the seizure onset zone and the pathways of seizure spread. Details of the surgical solution are also described.]
[Primary prevention program of the Hungarian Spine Society - Part I. Scientific background of the posture correction exercise scheme]
[The primary prevention program of the Hungarian Spine Society aims to increase awareness of the need to develop and automatically maintain a biomechanically correct posture for all school children. The biomechanically correct posture is a dynamic balance based on a correct middle position of the pelvis and on muscle balance. In this position three important anatomical points - the left and right anterior superior iliac spines and the upper medial point of the pubic bone - form one frontal plane. From side-view the imaginary weight median of the body crosses the 2nd to 5th lumbar and the 2nd to 5th cervical vertebral bodies. When the muscles involved in posture are in balance, their strength and flexibility are just appropriate for the almost continuous work required against gravity. In case of static and/or dynamic under- or overload tonic muscles become shortened, and phasic muscles become stretched, and are no longer able to work optimally. Since many muscles and muscle parts that are involved in normal posture maintenance are not satisfactorily challenged in regular physical exercises and sport activities, the preventive exercise scheme of the Hungarian Spine Society aimed to involve these rarely used muscles in special strengthening and stretching exercises. The scheme is based on 12 test exercises that assess the strength and flexibility of postural muscles. A person who is able to do all test exercises correctly has no problem with his or her muscle balance. In order to counteract the harm caused by sedentary lifestyle already in childhood, regular use of this posture correction scheme in physical education starting from preschool throughout the school-years is recommended for all children.]
[Volumetric changes following 125 I interstitial irradiation of low grade gliomas]
[Background - Image fusion permits quantitative analysis of the consequences of 125 Iodine interstitial irradiation of brain tumors. The volume of tumor necrosis, reactive zone and edema can be compared to the dosimetric data. Patients and method - Nineteen patients with low grade glioma were analyzed on the average 14.5 months following 125 Iodine interstitial irradiation. Dose planning and image fusion were performed with the Target 1.19 (BrainLab) software. The CT/MR images showing the so called “triple ring” (necrosis, reactive ring and edema) developing after the interstitial irradiation of brain tumors were fused with the planning images and the isodose curves. The volume of the three regions was measured. Values at the intersections of isodose curves and necrosis borders were averaged and used for calculation of tumor necrosis. The volume of normal brain tissue irradiated by given dose values, as well as homogeneity and conformality indices were also determined. Results - The relative volumes of the different parts of the “triple-ring” compared to the reference dose volume were the following: necrosis 54.9%, reactive zone 59.7%, and edema 445.3% . Tumor necrosis developed at 71.9 Gy dose. At the irradiation of an average size glioma with a volume of 12.7 cm3, 5 to 7 cm3 normal brain tissue around the tumor received 60-70 Gy dose. The average homogeneity and conformality indices were 0.24 and 0.57, respectively. Conclusion - The analysis of changes in the volume of edema, reactive ring and necrosis caused by interstitial irradiation, and their correlation with the dozimetric data using the image fusion method provide useful information for patient follow-up, clinical management and further therapeutic decisions.]
[Cognitive theory of psychotrauma and the medical psychotherapy]
[Cognitive theory of psychotrauma and the medical psychotherapy 2005;58(03-04)]
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey3.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries4.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]5.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]1.
Clinical Neuroscience Proceedings
[A Magyar Stroke Társaság XVIII. Kongresszusa és a Magyar Neuroszonológiai Társaság XV. Konferenciája. Absztraktfüzet]2.
3.
Journal of Nursing Theory and Practice
[A selection of the entries submitted to the literary contest "Honorable mission: the joys and challenges of our profession" ]4.
Journal of Nursing Theory and Practice
[End of Life and Palliative Care of Newborns in the Nursing Context]5.
Journal of Nursing Theory and Practice
[Aspects of Occupational Health Nursing for Incurable Patients ]