The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Specialities
Neurology
Personalized analysis of pain–weather associations: a pilot study
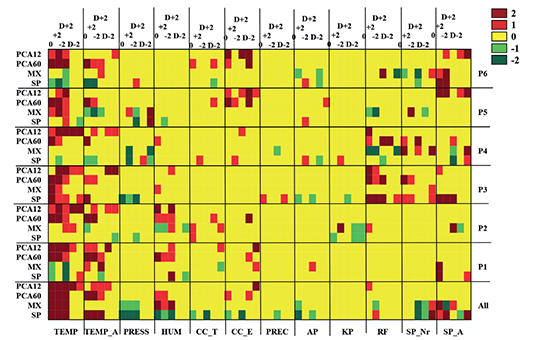
It is a wellknown belief that weather can influence human health, including pain sensation. However, the current data are controversial, which might be due to the wide range of interindividual differences. The present study aimed to characterize the individual pain–weather associations during chronic pain by utilizing several data analytical methods.
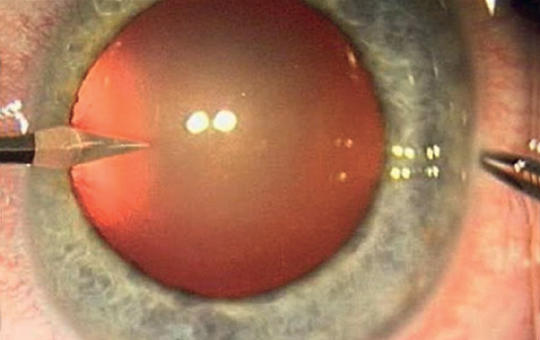
[Thrombolysis treatment and multi- disciplinary management of central retinal artery occlusion in comparison with traditional ophthalmological treatment options ]
[The management of central retinal artery occlusion (CRAO) has long been conservative therapy with limited efficacy carried out in ophthalmology departments together with etiological investigations lacking a standardised protocol. However, CRAO is analogous to ischemic central nervous system stroke and is associated with increased stroke risk, thus, systemic thrombolysis treatment and multidisciplinary management can be beneficial. Since May 2022, at Semmelweis University CRAO patients diagnosed within 4.5 hours are given intravenous thrombolysis therapy and undergo etiologic workup based on current stroke protocols. Here we report our experience with the multidisciplinary, protocol-based management of CRAO in comparison with former non-protocol based ophthalmological conservative treatment.
We reviewed CRAO patients’ data treated conservatively and with paracentesis within 6 hours at the Department of Ophthalmology between 2013 and 2022 including changes in visual acuity, neurological and cardiovascular findings compared to those in the thrombolysis project.
Of the 78 patients receiving non-protocol care, visual improvement was seen in 37% with natural course, 47% with conservative treatment and 47% with paracentesis. Four patients had significant carotid stenosis (2 underwent endarterectomy), 1 carotid dissection, 6 cardioembolism and 1 giant cell arteritis. Of the 4 patients within 4,5 hours, 3 gave their consent to the clinical trial and were treated with thrombolysis and underwent a full etiological assessment.
2 patients had improved visual acuity, 2 patients had significant carotid stenosis and underwent endarterectomy, 1 patient was started on anticoagulation for newly diagnosed atrial fibrillation.
CRAO patients presenting within 4,5 hours are rare and more patients are needed in our study to establish the efficacy of thrombolysis. However uniform protocollized evaluation helps identifying embolic sources thus, avoiding further and potentially more serious thromboembolic events.]
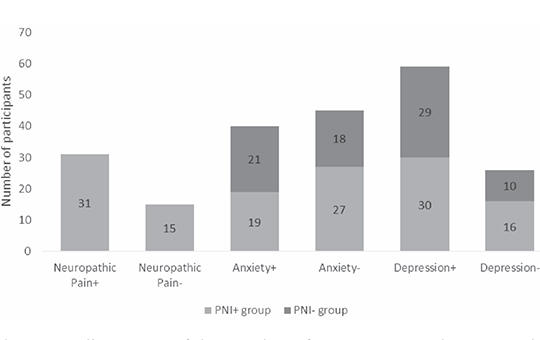
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries
Natural disasters, such as earthquakes, frequently result in mood disorders among affected individuals. It is established that neuropathic pain arising from traumatic neuropathies is also linked to mood disorders. This study investigates the influence of neuropathic pain on the development of mood disorders in earthquake survivors with peripheral nerve injuries, following the earthquake centered in Kahramanmaraş on February 6, 2023.
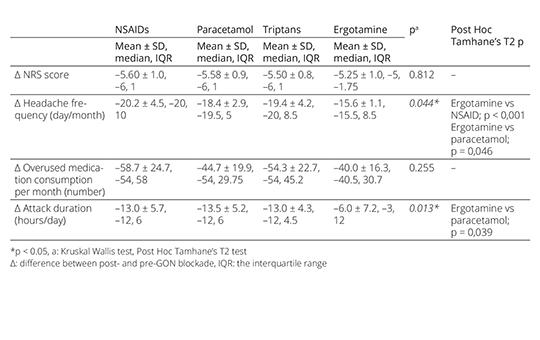
The effect of anesthetic blockade of greater occipital nerve during the withdrawal period of the medication overuse headache treatment
Discontinuation of medication still remains a key element in the treatment of medication overuse headache (MOH), but there is no consensus on the withdrawal procedure. We aimed to share the promising results of anesthetic blockade of greater occipital nerve (GON), which can be an alternative to existing treatments during the early withdrawal period of MOH treatment.
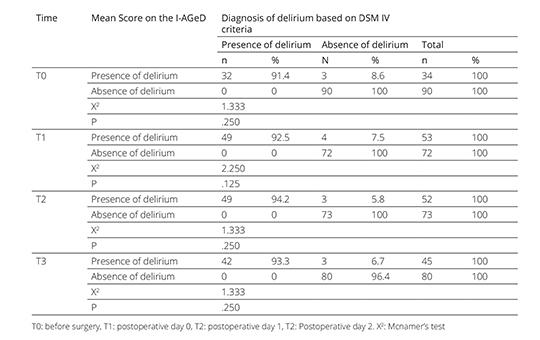
Validity and reliability of the Turkish version of the Informant Assessment of Geriatric Delirium Scale
Delirium is a common complication developing in elderly patients. Therefore, it is important to diagnose delirium earlier. Family caregivers play an active role in early diagnosis of delirium and build a bridge between health professionals and patients. The purpose of this research was to achieve the validity and reliability of the Turkish version of the Informant Assessment of Geriatric Delirium Scale (IAGeD).
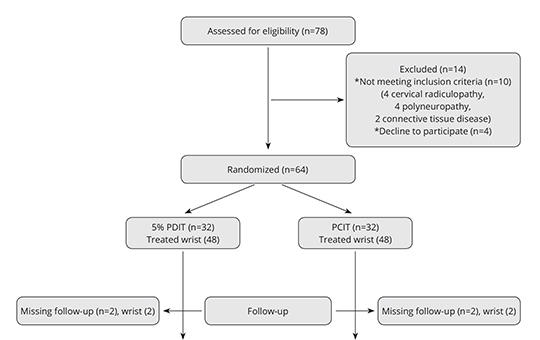
Perineural 5% dextrose versus corticosteroid injection in non-surgical carpal tunnel syndrom treatment
We aimed to investigate the difference of clinical and electrophysiological improvement between perineural corticosteroid injection therapy and perineural 5% dextrose injection therapy in carpal tunnel syndrome. Total of 92 wrists that were diagnosed as mild-to-moderate idiopathic CTS and completed their follow-up were included in our study. The severity of pain, symptom severity and functional status were assessed by visual analog scale.
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.