The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2005;58(01-02)
Content
[DIZZINESS - VERTIGO WARNING SYMPTOMS IN VERTEBROBASILAR ISCHEMIA PART II.]
[Dizziness and vertigo - like headache - are the most common complaints which lead patients to visit the doctor. In spite of the headache - which may be primary (e.g. migraine) or symptomatic - dizziness and vertigo do not appear to be a separate nosologic entity but rather the symptoms of several neurological disorders. For differential diagnosis, interdisciplinary thinking and activity is needed because the vestibular, neurological and psychiatric disorders might have a common role in the development of symptoms and further overlapping can also occur. The vascular disorders of the vertebrobasilar system are discussed in detail in this review. The importance, occurrence and causes of vertigo as a warning symptom is in the focus. The author draws attention to life-threatening conditions with acute onset in cases of the posterior scale ischemia and emphasizes the importance of the correct and early diagnosis. The author tries to clear up the nihilistic aspect in treating of stroke and stresses the necessity of thrombolysis and interventional radiological procedures which may be the only chance for the recovery of the patients. The pharmacological prevention of recurrent vascular events is also important and obligatory for the clinicians.]
[CHRONIC INFLAMMATORY POLYNEUROPATHIES]
[There is an increasing number of peripheral nerve disorders with inflammatory and immune mechanisms involved. The precise diagnosis is of utmost importance, since these patients can be successfully treated. Unfortunately, there is no specific marker for any disease of this group. The diagnosis therefore relies on the appropriate consideration of the clinical, neurophysiological and laboratory data, which requires in-depth knowledge of these diseases. In this paper we review the diagnostic criteria and treatment strategies for the major types of chronic inflammatory polyneuropathies.]
[THE PERISYLVIAN EPILEPTIC NETWORK A unifying concept]
[In this work the authors provide evidences for a unifying concept of the syndromes of benign focal childhood epilepsies, Landau-Kleffner syndrome, and electrical status epilepticus in sleep treating them as a spectrum of disorders with a common transient, age dependent, non lesional, genetically based epileptogenic abnormality, the nature of which is still not known. The electro-clinical features of these syndromes are congruent with the different degree involvement of the perisylvian cognitive network and with the involvement of the thalamo-cortical associative system of variable degree. These epilepsies are characterized by the abundance of regional epileptiform discharges in sharp contrast with the rare and in several cases lacking seizures. The nature and severity of interictal cognitive symptoms are closely related to localization within the network and amount of epileptic interictal discharges. Spike-wave discharges are attributed to an alternation of overexcitation (spikes) and overinhibition (waves). The recurrent overinhibition represented by the wave of the discharges may interfere with the continuous depolarization of the cells of a large population of neurons, which is a requirement of the overt seizures. The overinhibition also interfere with cognitive processes which are correlated with the continuous presence of the fast (gamma) activity, binding the required cortical areas. Hence the recurrent inhibition works against the existence of the binding fast frequency activity. This is the assumed reason for the co-existence of the relative lack of overt seizures and in the same time for the frequently observed epileptogenic cognitive deficit symptoms ("cognitive epilepsies"). The time course of these syndromes overlaps with important developmental milestones. The frequent epileptic discharges alters the evolution of the perisylvian network developing late after early childhood and is very vulnerable for any interference in this imprinting time for speech and other cognitive functions. This spectrum of disorders represents a type of age linked, mild to severe ‘epileptic encephalopathy’ limited to the perisylvian network, where the cognitive impairment is underlied by epileptic discharges interfering with cognitive development.]
[EXAMINATION OF NATURAL COAGULATION INHIBITOR PROTEINS IN THE ACUTE PHASE OF ISCHAEMIC ST]
[Introduction - Decreased activity of natural anticoagulants (antithrombin-III, protein C, protein S) rarely causes cerebral ischaemia, however it can be found frequently in acute phase of ischaemic stroke. The authors’ aim was to investigate whether the decreased activity of natural anticoagulants is accompanied by worsening of symptoms in ischaemic stroke. Patients and method - Sixty-eight acute ischaemic stroke patients were investigated. Severity of symptoms were assessed and followed by the NIH Stroke Scale. Antithrombin- III, protein C, protein S activities, and concentration of C-reactive protein (CRP) were measured within 48 hours after onset of ischaemic stroke. Results - Progressing stroke was found in 29% of patients. Decreased activity of at least one natural anticoagulant proteins was present in 31% of patients. Progression of stroke symptoms occured in 76% of patients with decreased natural anticoagulant activity, while this proportion was only 9% in those with normal natural coagulation inhibitor protein activity (p<0.01). Progressing stroke was also more frequent in patients with elevated CRP value (60%) than in those with normal CRP level (11%; p<0.05). Decreased activity of natural anticoagulants was more frequent in patients with elevated CRP concentration compared with patients with normal CRP. Conclusion - The results demonstrate the importance of decreased activity of natural anticoagulants in acute phase of ischaemic stroke. This abnormality was present in about 1/3 of stroke patients. The decreased activity of natural coagulant inhibitor proteins may play an important role in development of progressing stroke thus indicating unfavourable outcome.]
[EXPERIMENTAL DEMYELINATION CAUSED BY PRIMARY OLIGODENDROCYTE DYSTROPHY Regional distribution of the lesions in the nervous system of mice brain]
[Background and purpose - Heterogeneity of multiple sclerosis lesions has been recently indicated: In addition to T-cell-mediated or T-cell plus antibody-mediated autoimmune mechanisms (patterns I-II) two other patterns (III-IV) were described. Patterns III-IV are characterized by primary oligodendrocyte dystrophy, reminiscent of virus- or toxin-induced demyelination rather than autoimmunity. It was described more than 30 years ago that dietary application of a copper-chelating agent called cuprizone results in primary oligodendrocyte degeneration which is followed by demyelination. The aim of the present study was to examine the regional distribution of cuprizone induced oligodendrocyte dystrophy and demyelination in the nervous system of mice. Material a methods - Demyelination was induced in male weanling Swis-Webster mice by feeding them on a diet containing 0.6% (W/W) cuprizone bis(cyclohexanone)-oxalyldihydrazone (G. F. Smith Chemical, Columbus OH) for 8 weeks. Animals were sacrificed after 3, 7, 14, 27, 35, 56 days of cuprizone administration. Samples were taken from corpus callosum, anterior commissure, optic nerve, cervical spinal cord and sciatic nerve. Samples were examined by immunohistochemistry, in situ hybridization for myelin proteins and myelin protein mRNA-s, respectively. Conventional neuropathological stainings and electron microscopy was also performed. Results - Oligodendrocyte degeneration and demyelination followed a particular standard pattern in the central nervous system. Profound myelin loss developed in the superior cerebellar peduncle, anterior comissure and corpus callosum, whereas the optic nerves, velum medullare anterior and spinal cord showed little or no demyelination. Sciatic nerves were unaffected. No infiltration by lymphocytes or blood-brain barrier damage was observed during cuprizone treatment. Conclusion - Cuprizone induced oligodendrocyte damage and demyelination follows a particular standard pattern in the central nervous system of mice. Cuprizone induced demyelination might be considered as a model for human demyelinating disorders with primary oligodendrocyte dystrophy and apoptosis.]
[CLINICAL FEATURES OF CORTICOBASAL DEGENERATION]
[Corticobasal degeneration was described in 1968 by Rebeiz, Kolodny and Richardson, who characterized the disease as a syndrome of asymmetric akinesis and rigidity, dystonia of the upper limb, apraxia, myoclonus and dementia. Atrophy of the frontal and parietal lobe, neuronal loss, gliosis and achromatic neurones (and nowadays astrocytic plaques) are the characteristic pathological features of the disease. Corticobasal degeneration is a rare or a rarely recognized disease and it is frequently misdiagnosed as Parkinson’s disease. According to the Lang’s criteria, corticobasal degeneration can be diagnosed in the presence of rigidity and one cortical symptom (apraxia, cortical sensory loss, alien hand) or in a patient with rigidity, dystonia and focal reflex myoclonus. Exclusion criteria are early dementia (as in primary degenerative dementias), early vertical gaze problems (as in progressive supranuclear palsy), resting tremor and good, sustained therapeutic response to levodopa (as in Parkinson’s disease), severe autonomic problems (as in multiple system atrophy) and any pathology on imaging studies which might explain the clinical symptoms. It should be mentioned, that recently early dementia is recognized as an initial symptom of corticobasal degeneration. The authors present a case and review the literature to call attention to this disorder.]
[CALPAIN-3 GENE DEFECT CAUSING LIMB GIRD MUSCULAR DYSTROPHY IN A HUNGARIAN FAMILY]
[Limb gird muscular dystrophies (LGMD2) are a clinically and genetically heterogeneous group of hereditary diseases with autosomal recessive trait, characterized by progressive atrophy and weakness predominantly in the proximal limb muscles. The authors present clinical, histological, immunohistochemical and immunoblot results of two sisters suffering from so far unclassified autosomal recessive limb girdle muscular dystrophy. Haplotype analysis for genes possibly involved in autosomal recessive limb girdle muscular dystrophies was performed in the genetically informative family. All of the results pointed to a molecular genetic defect of the calpain-3 (CAPN3) gene. Direct sequencing of the CAPN3 gene revealed compound hetereozygous state for two mutations previously described in association with limb girdle muscular dystrophy, proving pathogenity. The authors would like to emphasize the importance of the above described combined strategy in diagnosing limb girdle muscular dystrophies.]
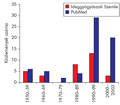
[The representation of headache in the Hungarian medical literature]
[Background - Less than 1.2% of papers published in the first 50 volumes of the journal Clinical Neuroscience/Ideggyógyászati Szemle - the major official journal of Hungarian neurologists - focused on headache despite the fact that headache is among the most frequent complaints in neurological consultations. In the current study the authors evaluated the presence of headache as the main topic in articles of the Hungarian medical literature. Methods - They identified full publications on headache by handsearching all volumes of the journal Clinical Neuroscience/ Ideggyógyászati Szemle from 1950 till the end of 2003. Electronic searches were performed to find Hungarian papers focusing on headache using the bibliographic databases of the Hungarian National Library of Healthcare (Hungarian Medical Bibliography, HMB) and the American National Library of Medicine of the National Institutes of Health (Medline and Oldmedline). Results of handsearch and electronic searches were cross checked for the journal Clinical Neuroscience/Ideggyógyászati Szemle. Results - Of the 2618 full papers published in Clinical Neuroscience/ Ideggyógyászati Szemle headache was the main topic in 32 articles (1.2%), most of them published after 1985. The electronic search of the HMB resulted in 132 documents in 41 journals, whereas using the PubMed search engine, they identified 66 Hungarian papers on headache. Migraine was the most frequent topic of interest in papers found by all three searches. The HMB search identified all headache articles published after 1990 in Clinical Neuroscience/Ideggyógyászati Szemle which were identified by handsearch. The Oldmedline, database contained four of the seven papers identified by handsearch from 1954-1964. After 2002, the start of indexing Clinical Neuroscience/Ideggyógyászati Szemle in the Medline, the only article identified by handsearch was also found by the electronic search. Conclusion - After the lack of interest until the mid-1980-ies, headache became a frequent topic in the Hungarian medical literature. Bibliographical data of articles on headache published after 1990 can be identified by electronic searches of the Hungarian and international bibliographic databases using carefully constructed but simple search strategies. An increasing presence of Hungarian headache research was found in international journals in the last two decades.]
[3rd International Scientific Symposium on Parkinson’s Disease]
[3rd International Scientific Symposium on Parkinson’s Disease 2005;58(01-02)]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.