Disaster is a sudden and unforeseen event that leads to catastrophic physical, economic and social conse quences for individuals. Such events may impose severe long-term effects on the physical and mental well-being of the affected population1. The earthquakes centered in Kahramanmaras/Turkey on February 6, 2023 resulted in a major catastrophe, causing over 50.000 deaths and more than 100.000 were injured. Natural disasters often contrib ute to the emergence of widespread mood disorders within affected populations. Existing literature indicates that vari ous factors including gender, age, educational level and physical damage are associated with the development of mood disorders in the aftermath of such events2–4.
Individuals trapped under debris in collapsed struc tures may sustain diverse injuries of their bodies and extremities, influenced by the location and duration of crush trauma. Such injuries may result directly from trauma, compression ischemia and compartment synd rome5, 6. Consequently, earthquake survivors may expe- rience peripheral nerve injuries (PNIs) alongside com monly observed damages such as crush syndrome, ex tremity fractures, pelvis and spinal injuries7–9.
PNIs cause varying degrees of sensorimotor losses and also impact the quality of life due to neuropathic pain (NP)10–12. Previous research has identified NP resulting from traumatic PNI as a significant risk factor for mood disorders13, 14. However, there is currently a gap in the literature regarding the specific investigation of the re lationship between mood disorders and NP in survivors with earthquake-related PNIs.
The primary objective of this study is to address this gap by hypothesizing that if NP resulting from traumatic neuropathy is an independent risk factor for mood dis orders, it may lead to more severe mood disorders in earthquake survivors with PNIs. Secondarily, we aim to examine and categorize the electrophysiological features of PNIs in earthquake survivors to elucidate the extent of neurological damage in the aftermath of a largescale disaster.
Methods
This singlecenter, crosssectional clinical study ana lyzed data from earthquake survivors aged 18 and above, who were referred to the neurophysiology laboratory of Adana City Training and Research Hospital between March 2023 and July 2023. The study received approval from the Ethics Committee of the University of Health Sciences Adana City Training and Research Hospital (Approval Number: 128/2628, 2023). Written informed consent was obtained from all participants.
Patients having electrophysiologically proven PNI associated with earthquake-related body and extremity damage were included in the study. The control group consisted of individuals without any physical injuries from the earthquake, including patient relatives and hos pital staff affected by the earthquake. Exclusion criteria for the study were as follows: 1) Having a pre-existing condition that would cause PNI (such as diabetes melli tus) before the earthquake, 2) Having traumatic neuropa thy unrelated to earthquake-related damage, 3) Having a pre-existing psychiatric disorder diagnosed before the earthquake.
A detailed trauma history was collected from all pa tients; documenting the presence of fractures, amputa tions, soft tissue injuries, compartment syndrome and crush syndrome in the body, along with any surgical in terventions. In the detailed neurological examination we assessed motor strength, sensory loss and deep tendon reflexes.
All electrophysiological examinations were conduct ed by the authors HCA and HF. The nerve conduction studies (NCS) and the needle electromyography (EMG) were performed using the Cadwell Sierra Summit EMG unit (Cadwell Laboratories, Kennewick, Washington, USA). Electrophysiological assessments were individu ally planned for each case, considering injury location, peripheral nerve structures susceptible to damage, and scar tissues in the extremities. Sensory and motor conduction of the median, ulnar, radial superficial, medial antebrachial cutaneous, and lateral antebrachial cutane ous nerves were evaluated in the upper extremities. In the lower extremities, motor and sensory conduction of the peroneal, posterior tibial, femoral, sural, superficial peroneal and saphenous nerves were assessed. The selec tion of muscles for needle EMG examination was based on neurological examination findings and abnormalities identified in NCSs.
In NCSs, a decrease or loss in compound nerve ac tion potential and/or compound muscle action potental amplitudes, slowing of nerve conduction velocity and the presence of conduction block were considered abnor mal. The presence of positive sharp waves and fibrilla tion potentials at rest and identification of early signs of regeneration were considered abnormal in needle EMG study15–17. Based on the obtained electrophysiological findings, the localization of the lesion was determined at the level of spinal roots, plexus or peripheral nerves18. If the electrophysiologically proven injury was limited to a single peripheral nerve (such as sciatic neuropathy), it was classified as a single nerve injury. Otherwise, le sions involving more than one nerve without fitting any specific plexus region or presenting with different lesions in different extremities (e.g., left brachial plexopathy and right sciatic neuropathy together) were defined as mul- tiple nerve injury.
In patients with PNI, NP was assessed using the Douleur Neuropathique 4 (DN4) questionnaire. The DN4 consists of 10 items divided into two subgroups: Patient Interview and Patient Examination, with a cut-off value set at four. If PNI was present in multiple extremities, patients were instructed to identify the extremity experi encing the most significant pain for assessment with the DN4 questionnaire19, 20.
Anxiety and depression levels in participants were as sessed using the Hospital Anxiety and Depression Scale (HADS). Subcategories, namely HADS-Anxiety (HADS-A) and HADS-Depression (HADS-D), were deemed abnor mal if their scores exceeded 10 and 7, respectively21, 22.
Statistical analyses were conducted us data between 3 or more groups. Correlation analysis was performed using either the Spearman or Pearson correla tion test, depending on the data distribution. Statistical significance was defined as p < 0.05.
Results
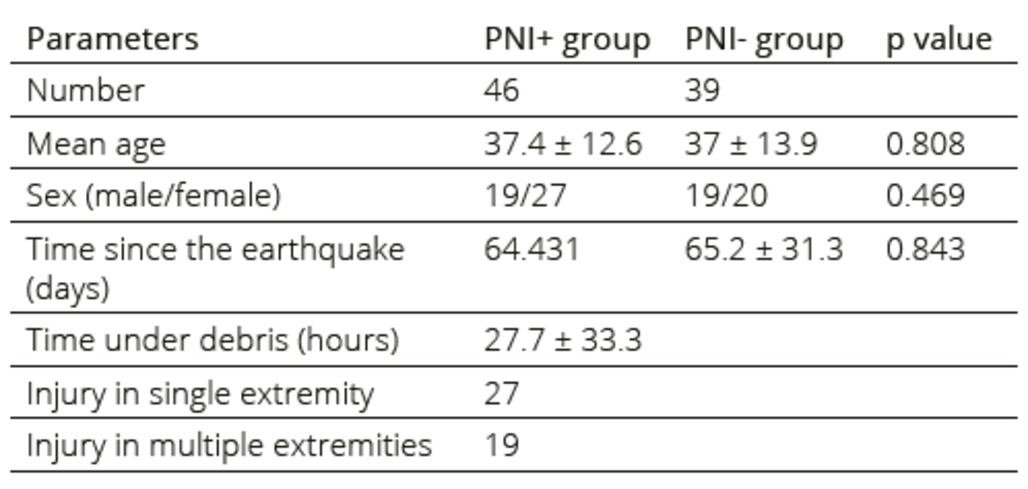
We reviewed the data of 46 earthquake survivors with peripheral nerve injury (PNI+) and 39 survivors without peripheral nerve injury (PNI-) as the control group. There were no statistically significant differences in terms of age (PNI+:37.4 ±12.6 vs PNI-:37±13.9; p˃0.05) and gender (PNI+: 19 male, 26 female vs PNI-: 19 male, 20 female) distribution between the groups. Table 1 presents a summary of the demographics and the data related to traumatic injuries.
Table 1. Demographics and injury related data of the participants
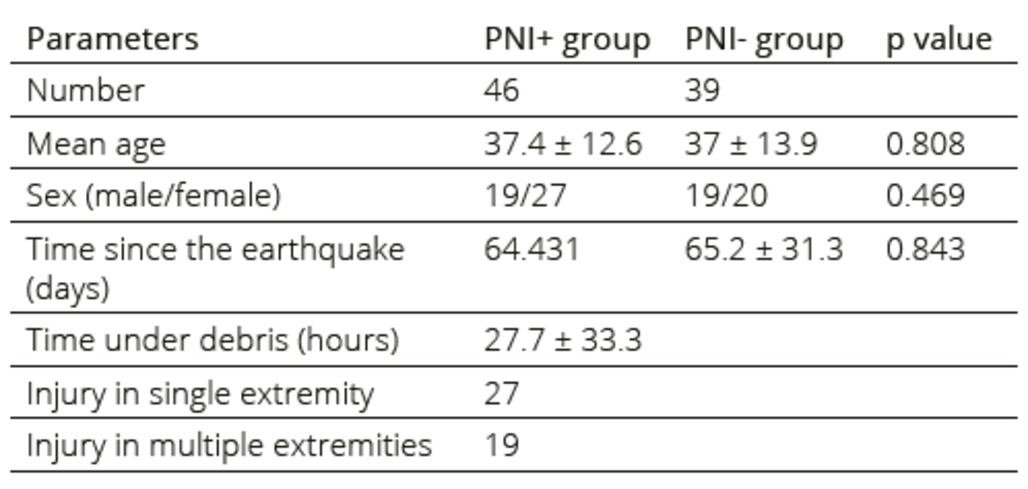
PNI: peripheral nerve injury
The most common injury in the upper extremities of PNI+ patients was ulnar neuropathy, while peroneal neuropathy was the most common injury in the lower extremities. The distribution of the damaged peripheral nerve structures is shown in Table 2.
Table 2. Distribution of peripheral nerve injuries

*Classification of injury based on lesion localization
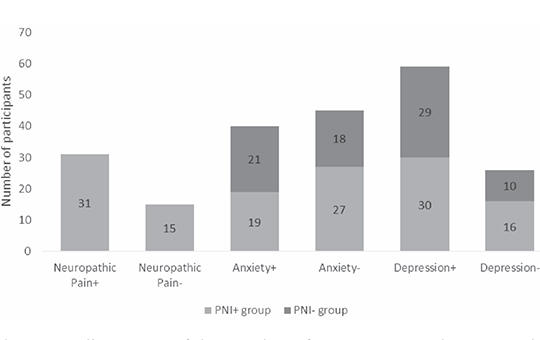
The average DN4 score in PNI+ cases was 5.2±1.8, indicating that 31 out of 46 patients in this group had NP. There was no significant difference between the PNI+ and PNI- groups regarding HADS-A (9.6±5.3 vs 9.4±4.4; p > 0.05) and HADS-D (10.6±5 vs 9.5±4.4; p > 0.05) scores. The number of abnormal HADS-A and HADS-D scores in the PNI+ group was 19 (41%) and 30 (65%), respectively; while in the PNI- group, it was 21 (53%) and 29 (74%), respectively. The Pearson Chi-Square test indicated no significant difference between the groups for both HADS-A and HADS-D scores (p > 0.05). Table 3 and Figure 1 summarize the results of applied scales.
Table 3. Results of the applied scales

DN4: Douleur neuropathique 4 questionnaire, HADS-A: hospital anxiety and depression scale anxiety subcategory, HADS-D: hospital anxiety and depression scale depression subcategory, PNI: peripheral nerve injury
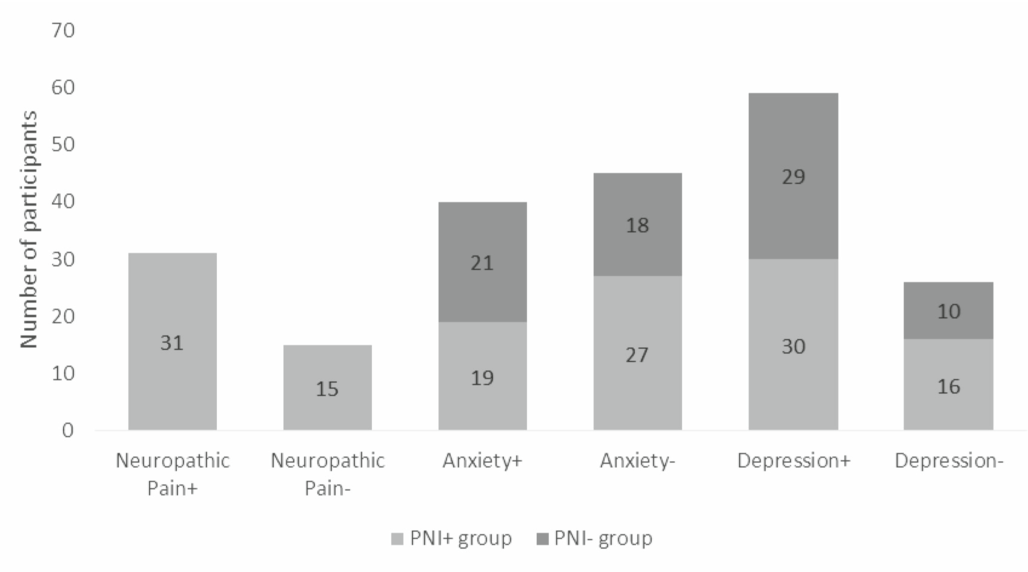
Figure 1. Illustration of the number of participants with neuropathic pain, anxiety and depression based on the results of DN4, HADS-A and HADS-D scales, respectively
PNI: peripheral nerve injury
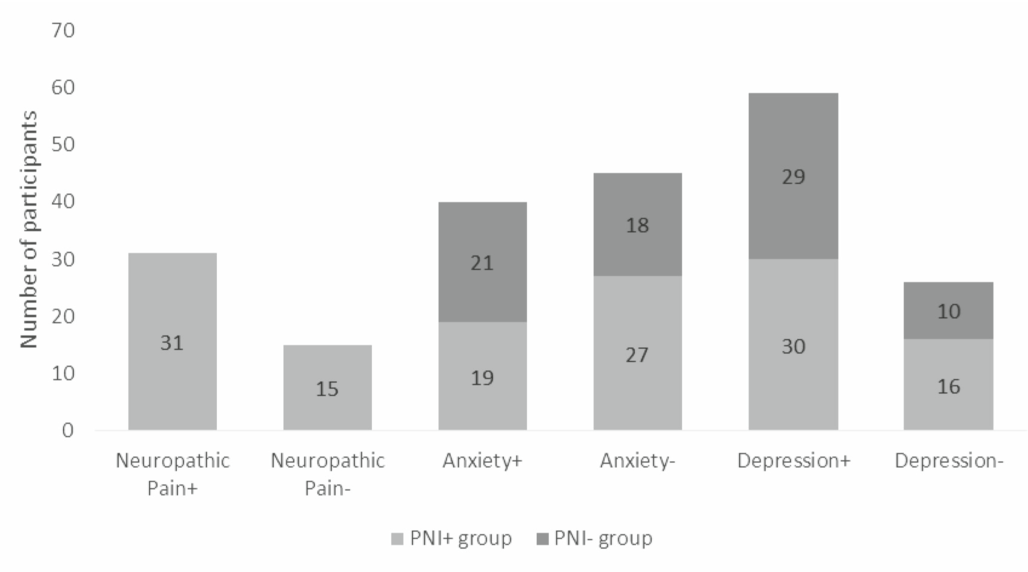
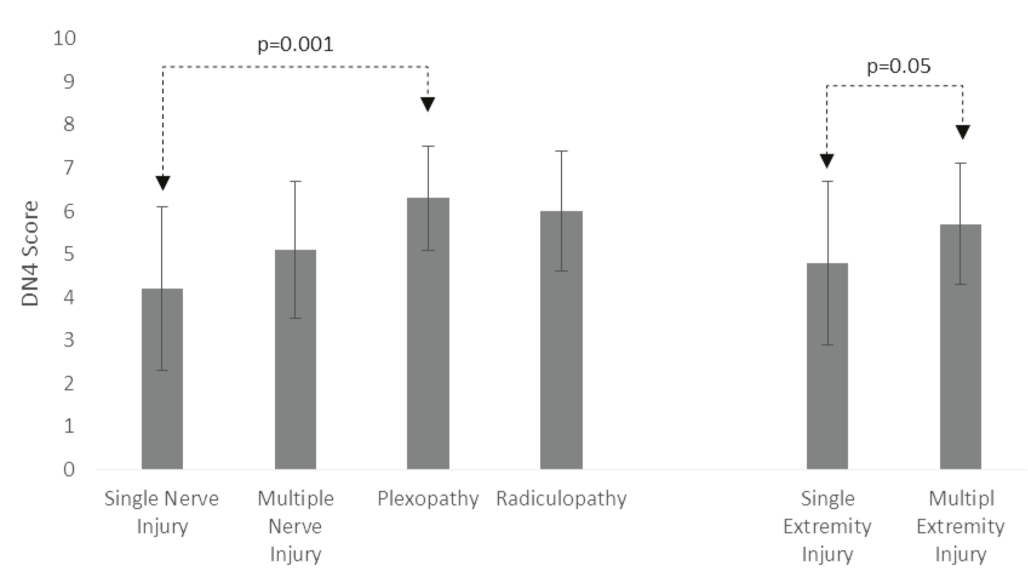
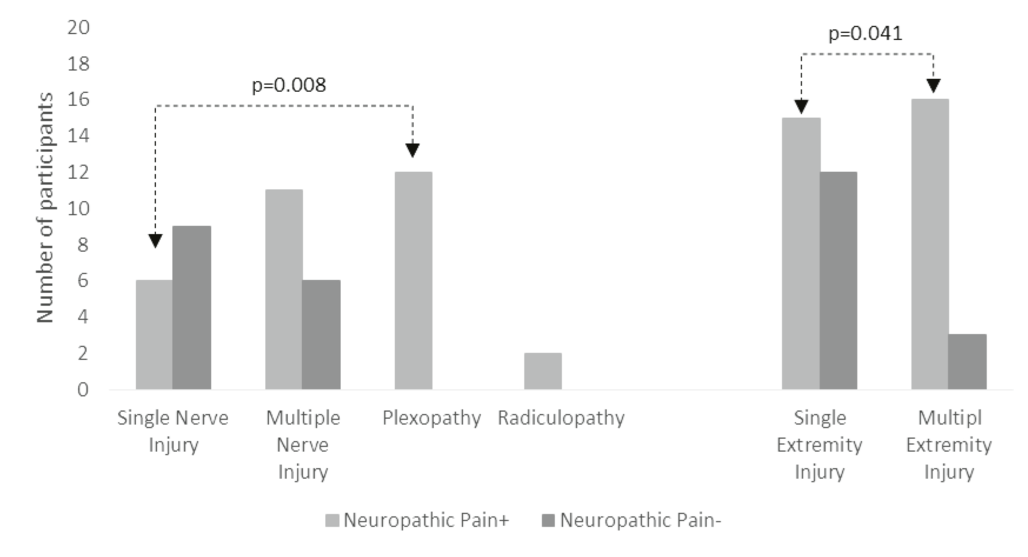
There was no significant association in PNI+ patients between the presence of NP, the number of affected extremities, the location of the damage in the upper or lower extremities and HADS-A or HADS-D scores. Upon evaluating based on lesion localization, we found that patients with plexopathy had significantly higher DN4 scores (6.3±1.2 vs 4.2±1.9; p=0.001) and a higher prevalence of NP (12/12 vs 6/15 p=0.008) compared to patients with single peripheral nerve damage (Figure 2). Moreover, patients with multiple extremity injuries were found to have more NP (16/19 vs 15/25; p=0.041) and higher DN4 scores (5.7±1.5 vs 4.1±1.9; p= 0.05) compared to those with single extremity injuries (Figure 3). Correlation analyses revealed a significant association between the duration of being trapped under debris and HADS-D scores (Spearman rho: 0.34, p=0.021) in PNI+ patients. Also, both groups demonstrated a significant correlation between HADS-A and HADS-D (Pearson correlation: 0.315, p=0.003) scores.
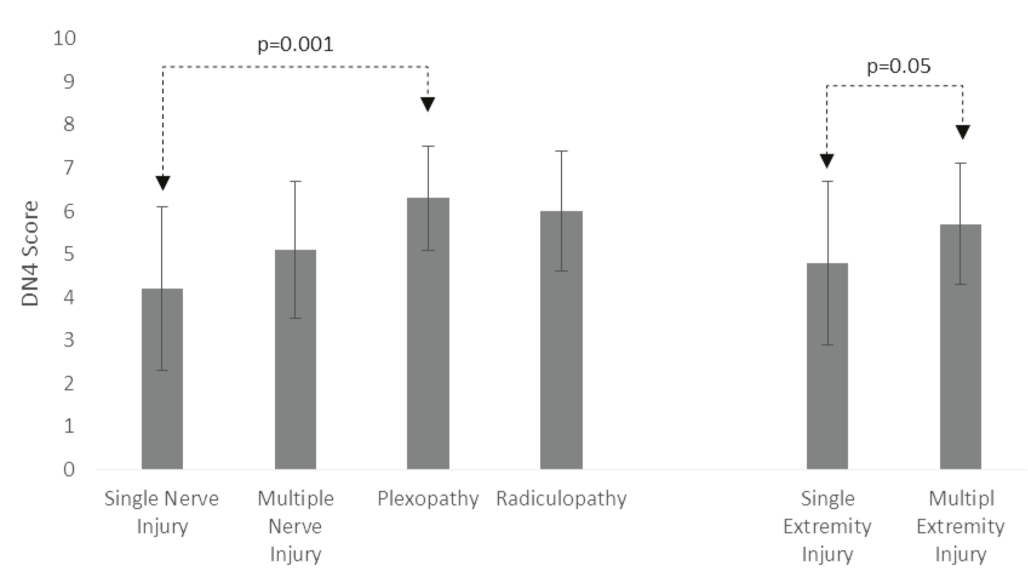
Figure 2. Results of DN4 scores based on the localization of the injury and the number of affected extremities
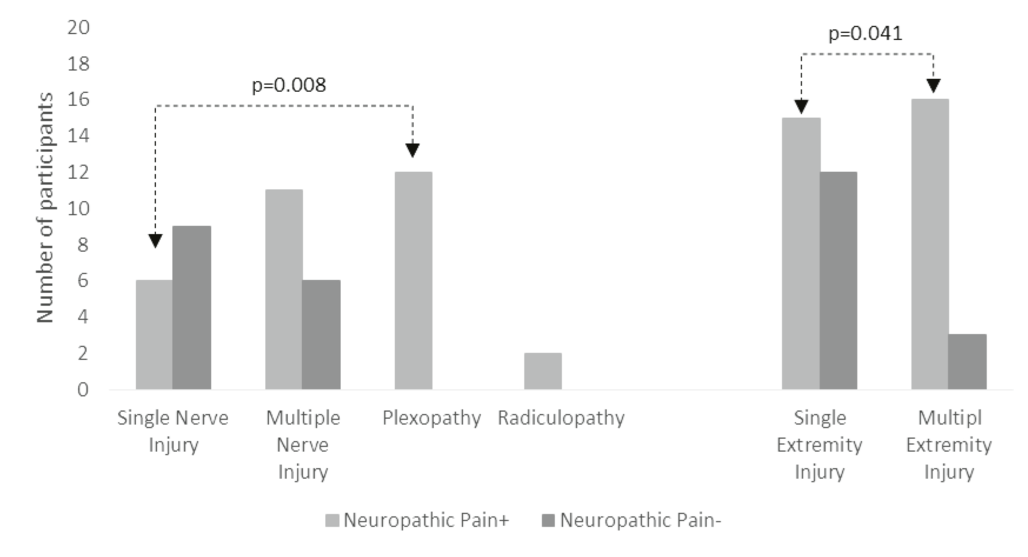
Figure 3. The number of cases with neuropathic pain based on the localization of the injury and the number of affected extremities
Discussion
To our knowledge, this study is the first to assess the relationship between PNI and mood disorders, such as anxiety and depression, in earthquake survivors. The findings shed light on the complex interconnections between physical trauma, NP and mental health outcomes following a natural disaster. Additionally, there is limited literature about the electrophysiological investigations in PNIs that occur following a large-scale earthquake7–9, 23, 24. We believe that our findings could be beneficial in contributing to the literature in this aspect.
Contrary to our hypothesis, we did not find a significant relationship between NP and levels of anxiety and depression. Additionally, we observed that the distribution or severity of PNI did not have a significant impact on mood disorders. The initial inference drawn from these findings is that mood disorders developing after a major disaster may have causes beyond physical traumas. However, it is important to note that the participants were evaluated at an average of approximately 65 days, which is a relatively early time frame for such a large-scale disaster. Considering the chronic nature of the injuries in earthquake survivors included in our study, there might be a potential divergence between these two groups in the long term.
The failure of our hypothesis could also be attributed to the potential contribution of other physical injuries when NP and PNI are relatively mild in earthquake survivors. Conditions such as amputations or internal organ injuries may independently influence anxiety and depression levels, thereby complicating the direct association we sought to establish. Therefore, the overall complexity of the physical trauma landscape may have obscured a clearer understanding of the specific relationship we aimed to explore.
The substantial correlation observed between anxiety and depression scores in both PNI+ and PNI- groups emphasizes the interconnected nature of these mood disorders following a natural disaster3, 4. This underscores the importance of comprehensive mental health interventions that effectively address both anxiety and depression as integral components of the post-earthquake recovery process. Furthermore, the correlation between the duration of being trapped under debris and higher depression scores emphasizes the enduring psychological consequences of prolonged entrapment. This finding underlines the need for targeted mental health support for survivors who endured extended periods of entrapment during the earthquake.
Our study revealed a higher incidence of PNI in the lower extremities compared to the upper extremities. This is consistent with reports on earthquake survivors of the 1999 Marmara earthquake, where lower extremities were more commonly affected7, 8. However, other studies have presented conflicting findings, suggesting a higher prevalence of damage to the upper extremities9, 23. Factors such as the timing of the earthquake during sleep and the materials used in home construction could contribute to these variations. Nevertheless, considering the presence of other variables that might influence the outcomes, making a definitive inference about the cause of this pattern is challenging based on the available data.
The frequent involvement of the peroneal and sciatic nerves along with the sacral plexus in lower extremity injuries may be related with crush/compression type of the trauma. On the other hand, injuries in the upper extremities, particularly brachial plexopathies, may also be associated with stretching trauma23. Hence, we can speculate that in addition to compression and penetrating trauma due to debris, stretching trauma might be a potential risk factor, especially during rescue operations. Furthermore, ulnar and peroneal neuropathies were more frequent than other neuropathies in upper and lower extremities. Along with the abovementioned explanation about the etiology, another cause may be that these nerves are more superficial than others and vulnerable to crush/compression trauma18. However, a definitive conclusion cannot be made as our study did not specifically investigate this aspect.
NP was defined as a common outcome of trauma related PNI10, 11, 13. Similarly, our results proved that a substantial portion of PNI+ cases have NP indicating the necessity for targeted interventions to address pain management and enhance the overall well-being of survivors12.
Survivors with brachial plexopathy and multiple extremity injuries exhibited higher levels of NP. Previous studies have indicated that plexopathies generally result in a poorer prognosis compared to isolated PNIs and the increased prevalence of NP in plexopathies may be associated with a slower recovery7, 23. Considering that earthquake survivors with multiple extremity injuries and plexopathies also endure more significant physical damage, it can be inferred that the prognosis for PNIs in these cases may be poorer, consequently increasing the likelihood of experiencing NP.
This study has several limitations. Firstly, it was conducted based on cases evaluated at a single center. Given the much larger number of individuals affected by disasters, caution is warranted in generalizing our findings to the entire population of disaster survivors. Additionally, participants were assessed approximately 65 days after the earthquake and the one-time evaluation may not allow for inferences regarding the long-term impact of trauma on anxiety and depression. Psychiatric examinations for diagnosing anxiety or depression disorders were not conducted in this study. It should be noted that the HADS is not suitable for diagnosing clinical anxiety and depression disorders; rather, it is practical for evaluating symptoms in clinical settings. Finally, this study focused on assessing PNIs in earthquake survivors; however, the potential contribution of other physical injuries (such as amputations or internal organ injuries) to mood disorders should be taken into consideration.
In conclusion, this study investigated the interaction between PNIs, NP and mood disorders in the context of earthquake survivors. While we did not identify a direct relationship between NP resulting from PNI and mood disorders, our findings indicate a high prevalance of anxiety and depression among survivors. Additionally, we evaluated PNIs in earthquake survivors from an electrophysiological perspective. Further research is essential to explore additional factors influencing these relationships and to develop interventions addressing the unique challenges faced by individuals with PNIs in the aftermath of natural disasters.