The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2010;63(03-04)
Content
[Differential diagnosis of atypical Parkinsonian syndromes]
[Atypical Parkinson syndromes are distinguished from idiopathic Parkinson disease by insufficient or missing response to dopaminergic replacement therapy and therefore they have significantly unfavorable prognoses. Early differential diagnosis is very important for the patient. It enables the therapist to give suitable consults, to avoid unnecessary or inappropriate therapy, which are not free of medication side effects and furthermore facilitates the selection of adapted symptomatically medical and physical measures of treatment. In case of future development of neuroprotective or causally therapy strategies correct diagnosis will allow an early start of therapy. The differential diagnosis separation of the three clinical pictures from the idiopathic Parkinson disease with clinical criteria might be difficult in the early stage of disease. Additional neuroimaging and nuclear medical investigations may support the clinical probable diagnosis.]
[Frontotemporal dementia or frontotemporal lobar degeneration - Overview of a group of proteinopathies]
[Frontotemporal dementia is the second most common early onset dementia after Alzheimer disease. Frontotemporal dementias are a complex group of dementias. The clinical diagnosis can be perplexing because of concurring psychiatric and neurologic syndromes. Frontotemporal lobar degeneration, the underlying pathology, represents an emerging group of proteinopathies. Genetic factors play an important part in the etiologies of dementias. This article overviews current defining characteristics of frontotemporal dementias known also as frontotemporal lobar degenerations]
[Numbers, counting and calculating problems in view of cognitive neurology]
[The ability to count and calculate is a human-specific skill comprised of understanding numeric values and categories and performing numerical operations; it is an acoustic-verbal symbolic activity that may be expressed in writing and understood by reading. The neuronal bases and precursors of cognitive systems have been supplied to mankind by the process of evolution. Abilities to create symbols (speech, visual letter and number symbols) must have played a decisive role in the emergence of man from the world of primates. Although counting and calculating problems are classified into numerous types, two main forms of dyscalculia have practical importance: the acquired one (the loss of learned knowledge) and the developmental one (the disturbance of the acquisition of arythmetical knowledge).]
[Vertigo - comorbidity with psychiatric disorders]
[Vertigo is one of the most common symptom and complaint in the clinical practice. The differential diagnosis can only be attained by a careful interdisciplinary way of thinking and activity, given the fact that the vestibular, neurological and psychiatric disorders - considered as pathogenic factors - are being present simultaneously in triggering the symptoms, and there can be overlaps between the certain pathological processes. The author deals with the co-morbidity of the vertigo and the psychiatric symptoms - anxiety, panic-disorder -, pointing out the common neurobiological and neurophysiological factors in the background of the symptoms, emphasizing the importance of the SSRI-s in the restoration of the serotonerg dysfunction.]
[Role of diagnosis of dyslipidemia in primary and secondary vascular prevention in a neurology department]
[Lipids have important functions in the human body, but high serum cholesterol level is an important risk factor for cardiovascular and cerebrovascular diseases. Prevention of stroke includes modifying risk factors, like dyslipidemias. Based on this theory, we examined in practice the possible role of a public care neurology and stroke department with a large patient turnover in vascular risk screening with regard to the diagnosis of hyperlipidemia. We reviewed all the medical records (irrespective of disease groups) of patients hospitalized in 2007 at Department of Neurology and Stroke Center of Szent János Hospital of the Municipality of the City of Budapest. Patients included in the study were classified into three groups: 1. those admitted with acute stroke; 2. those with a history of acute stroke, but without evidence of a novel cerebrovascular event; 3. no history and evidence of cerebrovascular disease during hospitalization. Our data show that 17.6% of patients was diagnosed with hyperlipidemia during hospital care, and another 18.5% was known to have elevated cholesterol levels. Altogether, 36.1% of the 1438 patients evaluated had hyperlipidemia. Known hypercholesterolemia was 18.4% in patients admitted for acute stroke, 26.9% in patients formerly (but not currently) treated for cerebrovascular disease, and 13.6% in the third group. Newly diagnosed elevated cholesterol levels had highest rate (22.6%) in former stroke patients (currently treated for other diseases); 20.4% in patients with acute stroke, and 13.2% in the third group. In the first two groups, the number of patients newly diagnosed with elevated serum cholesterol almost equaled to those with already known hypercholesterolemia. Based on our data, neurology departments have an important role in diagnosing hyperlipidemia and vascular prevention.]
[Movement analyzing devices for analyzing the actual state of patients with movement disorders]
[Movement analysis gives valuable information on the actual state of patients. Based on it, the early diagnosis and objective assessment of the progress of several diseases can be helped. Our research work has been focused on developing clinically applicable movement analyzing devices.]
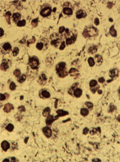
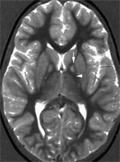
[Clinicopathological variability in neurodegeneration with brain iron accumulation]
[Neurodegeneration with brain iron accumulation (NBIA) is a rare, progressive neurodegenerative disorder with extrapyramidal and cognitive clinical symptoms characterized by iron accumulation predominantly in the globus pallidus, as well as extensive axonal spheroids in various regions of the brain. Recent studies indicate multiple genetic causes, however the illness can occur without obvious genetic background. The most frequent genetic form is the pantothene kinase associated neurodegeneration (PKAN) with mutation in the pantothenate kinase 2 (PANK2) gene. Further forms include phosphoslipase A2 (PLA2G6) gene mutation, neuroferritinopathy, and aceruloplasminaemia. To demonstrate the phenotypic variability associated with NBIA we present two patients. In the first patient iron deposition in the globus pallidus and axonal spheroids throughout the whole brain confirmed the neuropathological diagnosis of NBIA. Based on the long duration (27 years), the relatively late onset (at age of 13) of the disease, and the symmetrical hypointensity in the globus pallidus, without the eye-of-thetiger sign in cranial MRI, this case most likely represented an idiopathic form of NBIA but atypical PKAN may be also considered. In our second patient, who is still alive after duration of 9 years, MRI revealed the typical eye-of-the-tiger phenomenon that supported the clinical diagnosis of NBIA and was highly suggestive of PKAN. Since NBIA shows similarities with other neurodegenerative disorders, genetic examination may be essential in the diagnosis of this disease, however, cranial MRI together with the clinical picture may be highly indicative of NBIA.]
[Deep brain stimulation for treatment refractory obsessive-compulsive disorder - a case report]
[In the last 30 years it has been a great development in the understanding and therapy of obsessive-compulsive disorder. Adequate pharmaco- and cognitive-behavior therapies reduce the symptoms in 40-60% of patients, so a remarkable portion of patients still remains refractory to conventional treatment. Neurosurgery - with it’s reversible and irreversible techniques - brought a breakthrough in the therapy of treatment refractory patients. In the present case, we represent a 3 months follow-up of an obsessive-compulsive patient treated by deep brain stimulation. In our case, the stimulation target was the anterior limb of internal capsule. The clinical symptoms were measured by Y-BOCS. In addition various neuropsychological tests were used to monitor patient’s executive functions before and 3 months after the deep brain stimulation. We found that obsessive-compulsive symptoms improved after three months of the stimulation. The neuropsychological tests showed improvement in some executive functions (e.g. fluency, set-shifting, decision making). On the other hand our results revealed severe neurocognitive - mainly attention skill - deficits in a treatment refractory obsessive-compulsive patient.]
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey3.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries4.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]5.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]1.
Clinical Neuroscience Proceedings
[A Magyar Stroke Társaság XVIII. Kongresszusa és a Magyar Neuroszonológiai Társaság XV. Konferenciája. Absztraktfüzet]2.
3.
Journal of Nursing Theory and Practice
[A selection of the entries submitted to the literary contest "Honorable mission: the joys and challenges of our profession" ]4.
Journal of Nursing Theory and Practice
[End of Life and Palliative Care of Newborns in the Nursing Context]5.
Journal of Nursing Theory and Practice
[Aspects of Occupational Health Nursing for Incurable Patients ]