The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Lege Artis Medicinae - 2009;19(02)
Content
[Treatment of acute pancreatitis, with special regard to pharmaceutical therapy]
[Treatment of acute pancreatitis is mainly supportive, including the correction of any factors causing or sustaining the disease process, efforts to limit complications, as well as treatment of complications. Pharmaceutical efforts to influence the pathophysiological events with protease inhibitors or by influencing the release of the pro-inflammatory cytokine cascade did not prove to be effective, so there is no known effective and specific drug therapy for clinical use. Adequate pain control is an important component of pharmaceutical management, and - although yet controversial - early antibiotic prophylaxis and effective antimicrobial treatment of the inflammatory complications (infected necrosis or fluid collection, SIRS, sepsis) have probably a determining role in the outcome of severe necrotizing pancreatitis. Carbapenems proved to be the most potent antibiotics. For the prevention of the not infrequent fungal superinfection in acute pancreatitis, early administration of fluconasole can also decrease mortality. Surgery is indicated in the first stage of infected necrosis and infected pancreatic and peripancreatic fluid collections. In certain patients with a high operative risk, endoscopic or percutaneous drainage with lavage can also be worth trying. Optimal conditions for the treatment of severe necrotizing pancreatitis, as well as adequate management of multiple organ failure can only be warranted at an intensive care unit. In the chemoprevention of pancreatitis complicating endoscopic retrograde cholangiopancreatography (ERCP), non-steroidal anti-inflammatory drugs promise a new therapeutic option. There are insufficient data about the beneficial effects of the protease inhibitor ulinastatin, and results with nitroglycerin are contradictory.]
[Sudden cardiac death in athletes - cardiac electrophysiology point of view]
[Sudden cardiac death of athletes is very rare (1/50 000 to 1/100 000 annually) but it is still 2 to 4 times more frequent than that of the agematched normal population. In addition, it attracts peculiar media attention. Sudden cardiac death in athletes is supposed to not primarily have an ischemic origin but most likely relates to repolarization abnormalities. These may be caused by several independent and/or dependent factors such as benign cardiac hypertrophy developing normally in athletes (athlete’s heart), hypertrophic cardiomyopathy, increased sympathetic activity, genetic defects, seemingly harmless drugs, doping agents, food, and dietary supplements. These factors together can increase inhomogeneities in myocardial repolarization (“substrate”). In this case, an otherwise harmless extrasystole (“trigger”) occurring with unlucky timing may - although very seldomly - elicit fatal arrhythmias. Thus, effective prevention of sudden cardiac death may include new types of cost-effective cardiac electrophysiological screening methods (ECG or echocardiography) and, in case of a high level of suspicion, more costly genetic tests can be considered.]
[Practical considerations in the state-of-the-art management of ankylosing spondylitis]
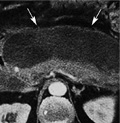
[Ankylosing spondylitis is an inflammatory rheumatic disease characterized by inflammation of the spinal and sacroiliacal joints, which causes chronic back pain and ultimately spinal stiffness, impaired motility, and deformity. Until the last decade, treatment mainly consisted of a combination of physical therapy and non-steroidal anti-inflammatory drugs, but recently tumor necrosis factor-α inhibitors revolutionized therapy and improved clinical outcomes. Tumor necrosis factor-α inhibitors effectively control inflammation of the sacroiliacal and spinal joints as shown by improved signs symptoms, and functions, magnetic resonance imaging findings, and reduction of acute phase reactants. Whether these drugs are capable of preventing radiographic progression and structural damage has, however, to be clarified in future studies. This review aims to highlight recent progress in the treatment of ankylosing spondylitis, and to provide recommendations for its management.]
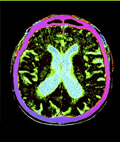
[Deep brain stimulation: a breakthrought in the treatment of movement disorders]
[Over the last 20 years, it became clear that deep brain stimulation is a breakthrough in the treatment of drug-resistant movement disorders. Stimulation acts by functional inhibition of certain pathologically hyperactive nuclei. Of advantage is that the patient himself can change stimulation parameters depending on his actual status, thus reaching optimal quality of life. This option has been available for years in Hungary, as well. It is a safe, effective and cost-effective alternative in the symptomatic management of drug-refractory Parkinson’s disease, essential tremor, and primary dystonia. Before surgery, a comprehensive investigation including clinical diagnosis, severity, surgery contraindications, and expected benefit has to be performed. Based on the results of international multicenter studies, bilateral subthalamic nucleus stimulation may improve - besides symptoms, such as tremor, rigidity, bradykinesia and levodopa-induced side effects - also quality of life in Parkinson’s disease. In essential tremor, stimulation of the ventral intermediate nucleus of the thalamus is capable of spectacularly decreasing tremor. For primary dystonias, stimulation of the pallidum can improve drug-resistant symptoms and quality of life, and it substantially reduces social dependency and the amount of nursing required. In childhood dystonias, surgery may be performed at an age of as low as seven years.]
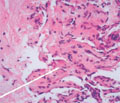
[Asymptomatic hepatic giant haemangioma]
[INTRODUCTION - Haemangioma is the most common type of benign hepatic tumors. Haemangiomas are usually asymptomatic, except for those that exceed five centimeters in size and are called “giant” haemangiomas. Malignant transformation has not been noted and therefore only regular follow-up is recommended for smaller haemangiomas. Surgical intervention becomes necessary only if symptoms or complications occur. Nevertheless, atypical presentation can cause a significant differential diagnostic problem. CASE REPORT - The authors report the case of a 51-year old woman with a focal hepatic abnormality diagnosed during a routine abdominal ultrasound examination. Results of the subsequent computed tomography scan suggested a multiple hepatocellular carcinoma based on the morphological appearance. Following oncology consultation, she was admitted to our department for liver biopsy. Histology did not reveal any malignancy. This result together with the lack of symptoms and complaints and the normal laboratory test results shifted the likely diagnosis towards a benign haemangioma. Blood-pool scintigraphy confirmed this diagnosis. CONCLUSIONS - Haemangiomas are benign hepatic tumors. They are often diagnosed accidentally, by routine abdominal ultrasound examination. If an abdominal ultrasound raises suspicion of haemangioma, abdominal MRI scan or blood-pool scintigraphy is recommended to be performed in order to exclude malignancy for lesion sizes of <2 cm or >2 cm, respectively. The reported case is considered important because of the differential diagnostic problems the large size and the atypical presentation of the given haemangioma imposed. Ultrasound-guided liver biopsy via fine-needle aspiration has previously been contraindicated. This invasive procedure can be performed in patients with focal hepatic pathology if diagnosis cannot be established by non-invasive tests, especially if malignancy is suspected. It can be performed conditional on the localization of the tumor, the patient’s general condition, the laboratory results, and if there is a therapeutic consequence of the biopsy results.]
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey3.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries4.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]5.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]1.
Clinical Neuroscience Proceedings
[A Magyar Stroke Társaság XVIII. Kongresszusa és a Magyar Neuroszonológiai Társaság XV. Konferenciája. Absztraktfüzet]2.
3.
Journal of Nursing Theory and Practice
[A selection of the entries submitted to the literary contest "Honorable mission: the joys and challenges of our profession" ]4.
Journal of Nursing Theory and Practice
[End of Life and Palliative Care of Newborns in the Nursing Context]5.
Journal of Nursing Theory and Practice
[Aspects of Occupational Health Nursing for Incurable Patients ]