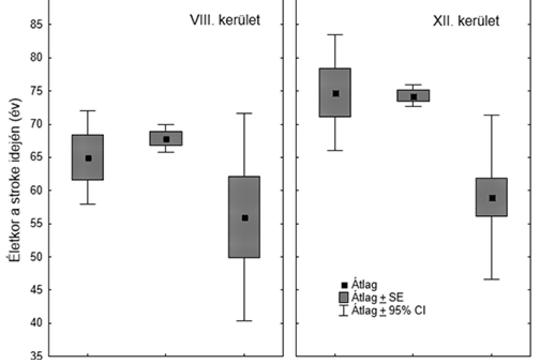
[The well-known gap between stroke mortality of Eastern and Western European countries may reflect the effect of socioeconomic differences. Such a gap may be present between neighborhoods of different wealth within one city. We set forth to compare age distribution, incidence, case fatality, mortality, and risk factor profile of stroke patients of the poorest (District 8) and wealthiest (District 12) districts of Budapest. We synthesize the results of our former comparative epidemiological investigations focusing on the association of socioeconomic background and features of stroke in two districts of the capital city of Hungary. The “Budapest District 8–12 project” pointed out the younger age of stroke patients of the poorer district, and established that the prevalence of smoking, alcohol-consumption, and untreated hypertension is also higher in District 8. The “Six Years in Two Districts” project involving 4779 patients with a 10-year follow-up revealed higher incidence, case fatality and mortality of stroke in the less wealthy district. The younger patients of the poorer region show higher risk-factor prevalence, die younger and their fatality grows faster during long-term follow-up. The higher prevalence of risk factors and the higher fatality of the younger age groups in the socioeconomically deprived district reflect the higher vulnerability of the population in District 8. The missing link between poverty and stroke outcome seems to be lifestyle risk-factors and lack of adherence to primary preventive efforts. Public health campaigns on stroke prevention should focus on the young generation of socioeconomically deprived neighborhoods. ]




COMMENTS
0 comments