The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2018;71(09-10)
Content
[Minimally invasive, extrapleural-anterolateral approach to the spine]
[In spine surgery, minimally invasive approaches (MIS) are getting accepted and more popular worldwide during the last decades. It is due to the reduced intraoperative blood loss, decreased infection rate, less postoperative pain and earlier discharge from hospital compared to traditional approaches. The present paper puts forward a minimally invasive extrapleural approach to the thoracic spine that is not applied in Hungary. This new approach, in contrast to the standard costotransversectomy, provides direct visual control over the ventral surface of the dural sac. Furthermore, contrary to the transthoracic way, following minimally invasive extrapleural surgery thoracic drainage and intensive care are not necessary. The approach can be applied safely in treatment of ventral or ventrolateral pathologies of the thoracic spine. ]
[28 years in the service of the cooperation of national clinical neurosciences]
[Two leading managers of the scientific journal currently publishing its 71st volume give an overview on the history and content- and form-related development of the journal. Recognizing the constantly decreasing role of paper-based literature products, the value system and the priorities of the journal were established more than 20 years ago: 1) preservation of high standards by achieving and maintaining international registration and annual qualification (i.e. impact factor); 2) enabling publication in Hungarian language for scientists living in Hungary and abroad; 3) displaying an ever broader spectrum of clinical neurosciences in the publications; 4) presentation of cutting-edge findings (related to the etiology, diagnostics, therapy, and care) of the most frequent and most relevant diseases in order to assure and enhance the quality of national clinical practice; 5) providing the possibility for the highest possible standard of scientific publication for Hungarian clinical neuroscientist; and finally 6) maintaining a readily available interaction surface and debate forum for the involved professionals in clinical questions of public interest. With respect to the above aspects, an outline is given of the efforts of the nearly three decades by listing editorial, publication, and other activities introduced throughout the history of the journal. The presumed strengths and weaknesses of the journal are summarized, the opportunities and limitations of the established objectives are highlighted, based on which the editors outline the most important tasks (SWOT analysis).]
[The evaluation of paroxysmal events in neonates and infants]
[Introduction - Differential diagnosis of neonatal and infantile seizures based only on inspection poses a challenge even for specialists. Aims - To investigate the evaluations of neonatal and infantile paroxysmal events based only on inspection. Research question - Is there any difference in the opinion of neonatologists, paediatric neurologists and neurologists about the assessment of common paroxysmal events in infancy? Patients and methods - Video recordings about paroxysmal movements of 15 neonates or infants (aged 2 days- 5 months) were displayed for 47 paediatric neurologists, 35 neonatologists and nurses working in Neonatal or Perinatal Intensive Care Units and 43 neurologists. They had to decide without knowing the past medical history or EEG results whether events presented were epileptic or nonepileptic in nature. Results - Answers of neonatologists and paediatric neurologists were correct in 67% of cases (824/1230), no significant difference was found between their results. The largest uncertainty was in the judgement of discrete hand movements and very rapid clonus with epileptic origin, they were judged correctly by only one third of participants. The result of neurologists was only slightly, but not significantly different from that of paediatric neurologists. Conclusion - In most cases, the correct diagnosis of neonatal and infantile paroxysmal events requires video-EEG recording. No significant difference was revealed between the evaluation of neonatologists and paediatric neurologists about the differential diagnosis of movements. The ongoing cooperation of paediatric neurologists and neurologists going back to several decades facilitates the shaping of a common perspective.]
[Diagnosis of multiple sclerosis: A review of the 2017 revisions of the McDonald criteria]
[The revolutionary progress of research in neuroimmunology has led to the introduction of disease modifying therapies in multiple sclerosis at the end of the last century. The International Panel on Diagnosis of Multiple Sclerosis originally proposed the 2001 McDonald criteria to facilitate the diagnosis of MS in patients with the first objective neurological symptom(s) suggesting demyelinating event, when magnetic resonance imaging is integrated with clinical and other paraclinical diagnostic methods. New terms have been introduced to substitute clinical information by MRI: dissemination in space - indicating a multifocal central demyelinating process and dissemination in time - indicating the development of new CNS lesions over time. The criteria for diagnosis of Multiple Sclerosis have continuously evolved, they were modified in 2005 and 2010 allowing for an earlier and more accurate diagnosis of MS over time, and they provided the most up-to-date guidance for clinicians and researchers. The last recommended revisions relied entirely on available evidence, and not on expert opinion thereby reducing the risk of the misdiagnosis. The 2017 McDonald criteria continue to apply primarily to patients experiencing a typical, clinically isolated syndrome. In this review, we provide an overview of the recent 2017 revisions to the criteria of dissemination in space and time with the importance of the presence of CSF-specific oligoclonal bands; keeping fully in mind that there is no better explanation for symptoms than diagnosis of MS. In the future, validation of the 2017 McDonald criteria will be needed in diverse populations. Further investigations are required on the value of new MRI approaches, on optic nerve involvement, on evoked potential and optical coherence tomography, in order to assess their possible contribution to diagnostic criteria.]
Anterior cerebral artery infarcts; two years follow-up study
Objectives – Anterior cerebral infarct (ACA) infarcts are reported very rare that is due to the compensatory collateral circulation provided by the anterior communicating artery. There are very few studies reporting the long-term follow-up results of ACA infarcts regarding their aetiology, clinical features and prognosis. Most studies reported in the literature vary between several months to one year. Patients and methods – A total of 27 patients with ACA infarcts were registered (14 women and 13 men). The mean age of the patients was 68.5 (age range: 45–89 years). Results – Bilateral ACA infarcts were reported in four patients (14.8%), right ACA infarct in 11 (40%) patients and left ACA infarct in 12 patients (44%). During the initial examination 15 patients (55.5%) were found to have apathy, 13 patients (48%) had incontinence, nine patients (33.3%) had primitive reflexes, 11 patients (40.7%) had aphasia, while six patients (22.2%) were found to suffer from neglect. At the end of one-year follow-up, five patients (22.7%) were reported to have apathy, 6 patients (27.2%) had incontinence, one patient (4.5%) had primitive reflexes, while one patient (4.5%) was found to have permanent aphasia, and no patients was found to suffer from neglect. Conclusion – Here we present our clinical data regarding the aetiology, specific clinical characteristics (including the speech disorders) and prognosis of 27 patients with ACA infarcts during a relatively longer follow-up period (3 months – 30 months) in compared to previous literature. We show that there are differences in the etiological factors of ACA infarcts between the Asian and European communities. Regarding speech disorders which are frequently reported during ACA infarcts, our study results are in agreement with other studies suggesting that this clinical picture is more than a real aphasia and associated with general hypokinesia and reduction in psychomotor activity.
A multidisciplinary clinical approach to facioscapulohumeral muscular dystrophy
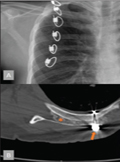
Background - Impaired shoulder function is the most disabling problem for daily life of Fascioscapulohumeral muscular dystrophy (FSHD) patients. Scapulothoracic arthrodesis can give a high impact to the functionality of patients. Here we report our experience with scapulothoracic arthrodesis and spinal stenosis surgery in FSHD patients. Patients and methods - 32 FSHD patients were collected between 2015-2016. Demographical and clinical features were documented. All the patients were neurologically examined. The Medical Research Council (MRC) and the FSHD evaluation scale was used to assess muscle involvement1. Scapulothoracic arthrodesis and spinal stenosis surgeries were performed in eligible patients. Results - There were 16 male and 16 female (mean age 34.4 years; range 12-73) patients. 6 shoulders of 4 patients aged between 2132 years underwent scapulothoracic arthrodesis (two bilateral, one left and one right sided). Only one 63 years old female patient with severe hyperlordosis had spinal fusion surgery. All of the patients undergoing these corrective surgeries have better functionality in daily life, as well as superior shoulder elevation. Conclusion - Until the emergence and clinical use of novel therapeutics, surgical interventions are indicated in carefully selected patients with FSHD to improve arm movements, the posture and the quality of life of patients in general. Scapulothorosic arthrodesis is a management with good clinical results and patient satisfaction. In selected cases other corrective orthopedic surgeries like spinal fusion may also be considered.
Caregiver burden and quality of life in early stages of idiopathic Parkinson’s disease
Objectives - The aim of this study was to assess the impact of early stage of idiopathic Parkinson’s disease (IPD) on caregiver burden with disease severity, duration, disability and psychiatric symptoms. Methods - 30 IPD patient (15 female, 15 male) - caregiver (18 female, 12 male) pairs participated in the study. Hoehn and Yahr (H-Y) scale was used to provide the assessment of disease progression and Unified Parkinson’s Disease Rating Scale (UPDRS) was used for assessing disability and impairment. Zarit Caregiver Burden Inventory (ZCBI) was used to ascertain the distress experienced by caregivers. Hospital Anxiety and Depression scale (HADS) was performed on both patient and caregiver groups to evaluate anxiety and depression. Depressive symptoms of both groups were also measured by Beck Depression Inventory (BDI). Patients’ psychotic symptoms were assessed using the part 1- mentation, behavior and mood section of UPDRS. Mini-Mental State Examination (MMSE) was used to evaluate dementia symptoms and Short Form-36 (SF-36) was also used to assess quality of life. Results - We found significant correlation between caregiver burden with disease severity and duration. There was a significant difference between high UPDRS scores and the caregiver’s will for placing her/his patient in a long-term institution. Patients who had depression risk according to BDI had also high UPDRS scores. Patients with off period had higher UPDRS scores and lower SF-36 subdomains of general health, physical functioning, emotional role and social functioning. Conclusion - IPD is a chronic, progressive neuro- degenerative disease and comprises substantial burden on patients, families of patients and caregivers. The disease duration and disability have a remarkable impact on caregiver burden. For the good quality of caregiving, protective therapies should be recommended for caregivers if needed.
Acute motor and sensory axonal neuropathy associated with Sjögren’s syndrome
Sjögren’s syndrome (SS) is an autoimmune disease with mononuclear cell infiltration and destruction of the lacrimal gland and salivary glands, which cause dryness of the eyes and mouth. The most common neurological condition seen in SS is peripheral neuropathy. Initial manifestation of SS as an acute fulminant peripheral neuropathy is extremely rare. We report a 42-year-old patient presenting with acute motor sensory-axonal neuropathy in the presence of SS. She showed partial response to intravenous immunoglobulin but favourable clinical improvement was seen after initiation of corticosteroid treatment.
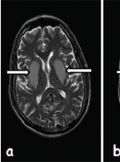
A rare condition mimicking stroke: Diabetic uremic encephalopathy
Uremic encephalopathy (UE) is a metabolic disorder associated with acute or chronic renal failure. It is characterized by the acute or subacute onset of reversible neurological symptoms and specific imaging findings. It is uncommon for uremic encephalopathy to be associated with acute bilateral lesions of the basal ganglia in diabetic uremic patients, and this can be seen most often in Asian patients. Here, we report a patient with diabetic uremic encephalopathy and bilateral basal ganglia lesions who developed acute onset dysarthria. The clinical and magnetic resonance brain imaging findings resolved after hemodialysis treatment.
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey3.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries4.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]5.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]1.
2.
Clinical Neuroscience Proceedings
[A Magyar Stroke Társaság XVIII. Kongresszusa és a Magyar Neuroszonológiai Társaság XV. Konferenciája. Absztraktfüzet]3.
4.
Journal of Nursing Theory and Practice
[A selection of the entries submitted to the literary contest "Honorable mission: the joys and challenges of our profession" ]5.
Journal of Nursing Theory and Practice
[End of Life and Palliative Care of Newborns in the Nursing Context]