The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Lege Artis Medicinae - 2022;32(01-02)
Content
[Cardiovascular prevention 2021 – Guidelines of European Society of Cardiology 2021. Prevention at the population level And Disease specific cardiovascular prevention]
[In our four-part publication we review the current state of cardiovascular prevention based on the European Society of Cardiology Guidelines 2021. In part 1 we reviewed the risk factors, risk assessment, age-specificities, the influencing factors, including diabetes mellitus and chronic kidney disease. In part 2 we concerned comorbidities affecting the cardiovascular risk. In part 3 we reviewed the personalised cardiovascular prevention and the management of specific risk factors, including optimisation of life style factors, management of lipid levels and high blood pressure and antithrombotic therapy. This part 4, we review the community level preventive measures (physical activity, diet, smoking habits and alcohol consumption) and the importance of governmental and non-governmental interventions. We provide a brief summary about the principles of cardiovascular prevention in individuals with coronary artery disaese, heart failure, cerebrovascular diseases, lower extremity artery disaese, chronic kidney disease, atrial fibrillation, and in multimorbid patients.]
[Main features of cardiovascular rehabilitation in post-acute Covid-19]
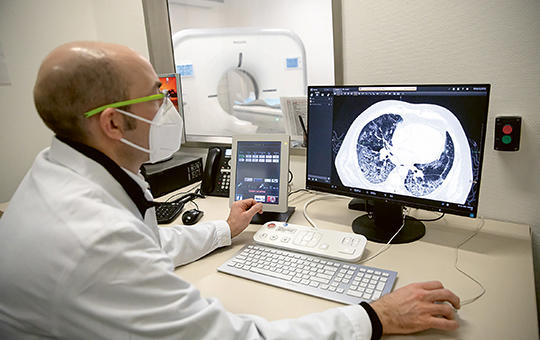
[The COVID-19 pandemic caused by SARS-CoV-2 is a significant challenge worldwide. Cornerstones of in-patient management of this pandemic which harms predominantly the respiratory system are the acute and intensive care. However, the rehabilitation plays a key role in improving the functional status and quality of life of survivors and reducing the impact of complications. As estimated, 40-50% of discharged patients require some form of medical support and 4-5% of them require inpatient rehabilitation. In addition to the respiratory system involvement, cardiovascular effects caused by COVID-19 (heart failure and myocarditis, acute coronary syndrome, arrhythmia, venous thromboembolism) are part of the ongoing systemic inflammatory processes and may affect 7-28% of hospitalized patients and lead to long-term deterioration in quality of life and loss of work capacity. Based on available scientific databases, expert consensus and the recommendations of European professional societies, this summary presents the recommended method, conditions and intensity of post-Covid cardiac rehabilitation including physical training exercises. The summary concerns also the recommended conditions for return to work and sporting activities. Structured exercise training is a very important and low-risk component of cardiac rehabilitation, reducing cardiovascular complications, thromboembolic complications, systemic inflammation and mortality, improving functional recovery and endothelial function. The planning of physical training should be preceded by a complex assessment of patients. Assessments of risk, capacity and function are needed to select the intensity, frequency and mode of individualized training. This should be combined with appropriate secondary preventive medication, monitoring, diet therapy and psychotherapy in accordance with respected principle of gradual progression. Finally, the consensus recommendations suggest that home-based and tele-rehabilitation should play a prominent role, considering the epidemiological and capacity constraints that also affect rehabilitation. ]
[Non-alcoholic fatty liver disease]
[Non-alcoholic fatty liver disease is estimated to affect 25% of the global population. It is often joining other metabolic disorders and features a heterogeneous natural history. Significant liver injury is unlikely to develop from steatosis, while a third of steatohepatitis cases will progress into cirrhosis and as a severe complication may lead to primary liver cancer. The probability of these severe outcome increases with the degree of liver fibrosis and with the prevalent type 2 diabetes and two or more metabolic risk factors. Regardless of its stage, non-alcoholic fatty liver disease is increasing the susceptibility for cardiovascular diseases, diabetes and all malignancies, and as a result is shortening the life expectancy. However, general awareness of the disease among healthcare professionals and their patients remains limited. Lack of approved medications for the disorder is likely a major contributor to this discrepancy. Since the disease primarily stems from sustained caloric excess, lifestyle modification including Mediterranean type diet, avoidance of alcohol consumption, and regular physical activity are the mainstay of management. Better education campaigns may improve patient compliance and enhance the recognition and acceptance of this condition within primary care, in parallel with the introduction of two-step fibrosis screening to achieve more efficient identification and management of the high-risk patients. ]
[Options for assessing the quality of postoperative pain relief: unidimensional scales]
[The measurement of the quality of postoperative pain relief receives increasing attention in clinical practice since the not properly treated pain has several negative consequences for both the patients and the health care providers. An important component of the evaluation of the quality of care is the measurement of patient outcomes, which needs regular pain assessments and reliable pain assessment tools. The main goal of our paper is to review the literature on scales and pain assessment tools for postoperative pain assessment, the systematic literature search of which was performed by the PICO (population, intervention, control, and outcomes) technique. We found 396 accessible and evaluable articles in total, and out of them we summarized the results of the most important 31 in English and 3 in Hungarian. Organisations in the field of pain relief recommend the regular assessment of postoperative pain by unidimensional and multidimensional scales. Among unidimensional scales, we compared the Numerical Rating Scale (NRS), the Visual Analogue Scale (VAS) and the Verbal Descriptor Scale (VDS) with one another by discussing their advantages and limitations in measuring the intensity of postoperative pain. Although in clinical practice NRS is the most widely used one, VAS is more sensitive in the detection of changes and the best for statistical analysis. The advantage of VDS is that no significant differences can be detected in the interpretation of its results. At the same time, the application of VAS is the most difficult and the least preferred by patients and not always applicable immediately after the operation. The VDS is the least sensitive measurement tool, whose results are influenced by differences of the patients’ verbal interpretation, thus it is not applicable among patients with a weak vocabulary. In general, the main advantage of unidimensional scales is that they are fast and easy to use, but they measure only one dimension of pain, namely its intensity, and the association between the intensity ratings, the patients' subjective experience of pain and its observable consequences are not unequivocal in certain cases. Consequently, when the circumstances permit, the use of multidimensional measurement tools should be considered.]
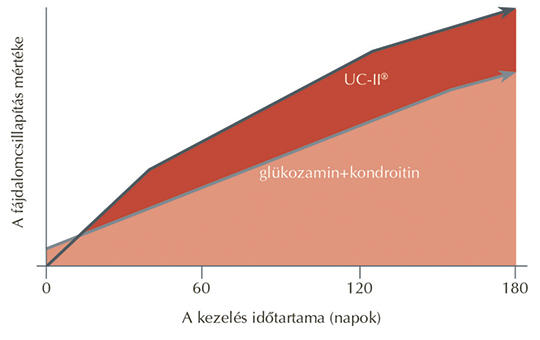
[Paradigm shift in the treatment of osteoarthrosis and the importance of prevention today]
[Osteoarthrosis is a major burden on our society, both in terms of health affairs and health economy. The increasing strain on joints by competitive sports and the growing prevalence of sedentary lifestyle are coupled main factors behind the increasing occurence of osteoarthritis in younger generations. Its pathomechanism is recently recognised to be a combination of inflammatory and degenerative processes. Concerning the serious and even quality of life worsening outcomes and its growing and spreading prevalence, the role of prevention has become crucial. This study reviews the preventive options, emphasizing the importance of recreational sport and physical activities, while presenting also the new generation of chondroprotective agents. ]
[Telephone based supporting program to quit tobacco smoking in Hungary]
[The National Korányi Institute of Pulmonology, Methodology Centre for Tobacco Smoking Cessation Support has been operating a free quitline since 2013. The aim of the program is to provide professional advice on how to quit smoking, to spread information about supporting services and to refer interested smokers to specialized health care providers. Proactive calls following a specific protocol are available once a week for a six week period. This study presents the activities of our service in the last six years. Data of our retrospective longitudinal study were analysed by descriptive statistical methods. Between 2015 and 2020, there were received 24 286 messages received on the answering machine of the quit-line service. We were able to initiate conversation with approximately 55% of the interested callers. The free of charge quit-line is used predominantly by lower educated and indigent people. Program participants had a serious nicotine addiction. The program is particularly useful for smokers who are otherwise less likely to receive expert support. Between 2015 and 2020, the average abstinence rate of program participants was 16% after their proactive calls. The initial abstinence rate was 19% in 2015, which dropped to 6% in 2020. In this period the average quit rate was 13% at the six-month and 9% at the one-year follow-up. One possible reason for the low cessation rate is that the telephone counselling program can focus only on changing the patients’ behaviour without the in-person help of pharmacological support. Thus healthcare workers play a key role in encouraging of quit smoking and managing the nicotine withdrawal.]
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey3.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries4.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]5.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]1.
Clinical Neuroscience Proceedings
[A Magyar Stroke Társaság XVIII. Kongresszusa és a Magyar Neuroszonológiai Társaság XV. Konferenciája. Absztraktfüzet]2.
3.
Journal of Nursing Theory and Practice
[A selection of the entries submitted to the literary contest "Honorable mission: the joys and challenges of our profession" ]4.
Journal of Nursing Theory and Practice
[End of Life and Palliative Care of Newborns in the Nursing Context]5.
Journal of Nursing Theory and Practice
[Aspects of Occupational Health Nursing for Incurable Patients ]