The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2012;65(09-10)
Content
[Burning sensation in oral cavity - burning mouth syndrome in everyday medical practice]
[Burning mouth syndrome (BMS) refers to chronic orofacial pain, unaccompanied by mucosal lesions or other evident clinical signs. It is observed principally in middle-aged patients and postmenopausal women. BMS is characterized by an intense burning or stinging sensation, preferably on the tongue or in other areas of the oral mucosa. It can be accompanied by other sensory disorders such as dry mouth or taste alterations. Probably of multifactorial origin, and often idiopathic, with a still unknown etiopathogenesis in which local, systemic and psychological factors are implicated. Currently there is no consensus on the diagnosis and classification of BMS. This study reviews the literature on this syndrome, with special reference to the etiological factors that may be involved and the clinical aspects they present. The diagnostic criteria that should be followed and the therapeutic management are discussed with reference to the most recent studies.]
[Administration of preemptive analgesia by diclofenac to prevent acute postcraniotomy headache]
[Purpose - Postcraniotomy headache (PCH) is a frequent perioperative complication in neuroanesthesia. The aim of the present work was to assess the incidence of PCH and to test the efficacy and safety of preoperatively administered diclofenac. Methods - Patients undergoing craniotomies for intracranial tumor resections were enrolled. In the case group 100 mg diclofenac p.o. one hour prior to surgery was used as a preemptive analgesic along with infiltration of the surgical site with a combination of lidocaine and epinephrine. In controls only surgical site infiltration was used. VAS scores were assessed preoperatively, on the day of surgery (DoS), on the 1st and 5th postoperative days. Results - We have found that PCH of any severity is between 50-90% during the first five days after surgery. The number of cases characterized as “no pain” significantly decreased in the early postoperative period, but remained in both groups still higher on the 5th postoperative day than observed preoperatively. In both groups, the number of headaches characterized as mild pain remained relatively stable and substantial increases in case numbers were observed in moderate and severe headaches, showing a declining tendency over time in the postoperative period. A significant effect of diclofenac pretreatment was observed compared to controls on DoS (χ2: 10.429, p<0.015), on the 1st (χ2: 8.75, p<0.032) and 5th postoperative days (χ2: 14.3, p<0.002). Conclusions - The relatively low incidence of severe PCH on day five in the diclofenac group may indicate that preoperatively administered diclofenac effectively reduces postcraniotomy headache. A randomized study is encouraged to test this hypothesis.]
[A prospective study evaluating the clinical characteristics of cluster headache]
[Introduction - Although cluster headache (CH) is one of the most severe human pain syndromes, its symptoms and therapeutic possibilities may be suboptimally recognised in current medical practice in Hungary. Aim - To present the clinical characteristics of CH based on a prospective study of patients attending the Headache Service of the Department of Neurology, Semmelweis University. Methods - We collected information about the symptoms, diagnosis and previous treatment of CH patients by filling in a 108-item questionnaire during outpatient visits. Results - In the 5-year period between 2004 and 2008 we obtained data from 78 CH patients (57 males and 21 females; mean age: 44.6±14.6 years). The male:female ratio did not change in subgroups based on disease onset (calendar years). Ninety-three percent considered CH the most severe pain state of their life. The pain was strictly unilateral, affecting the territory of the 1st trigeminal division in all patients. The attacks were accompanied by signs of ipsilateral cranial parasympathetic activation (lactimation 83%, conjunctival injection 67%, rhinorrhea 56%, nasal congestion 43%); less frequently, signs of sympathetic dysfunction (ptosis 48%, miosis 7%) were also present. Two patients had attacks showing the typical localisation, severity and time course of CH attacks, but not accompanied by autonomic phenomena. A considerable part of the patients also observed symptoms that are usually ascribed to migraine (nausea 41%, vomiting 18%, photophobia 68%, phonophobia 58%). This may have been instrumental in the fact that, regardless of the characteristic clinical symptoms, the diagnosis of CH took 10 years on average. At the time of their examination 63% of patients were not using adequate abortive medications and 59% did not have an adequate prophylactic measure. Discussion - Cluster headache is characterised by attacks of devastating pain that warrant an early diagnosis and adequate treatment. Our study underlines that information about the diagnosis and therapy of CH should be emphasized on occasions of neurology specialty training and continuing medical education.]
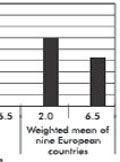
[Health status and costs of ambulatory patients with multiple sclerosis in Hungary]
[Background and purpose - Data on disease burden of multiple sclerosis from Eastern-Central Europe are very limited. Our aim was to explore the quality of life, resource utilisation and costs of ambulating patients with multiple sclerosis in Hungary. Methods - Cross-sectional questionnaire survey was performed in two outpatient neurology centres in 2009. Clinical history, health care utilisation in the past 12 months were surveyed, the Expanded Disability Status Scale and the EQ-5D questionnaires were applied. Cost calculation was conducted from the societal perspective. Results - Sixty-eight patients (female 70.6%) aged 38.0 (SD 9.1) with disease duration of 7.8 (SD 6.7) years were involved. Fifty-five (80.9%) had relapsing-remitting form and 52 (76.5%) were taking immunomodulatory drug. The average scores were: Expanded Disability Status Scale 1.9 (SD 1.7), EQ-5D 0.67 (SD 0.28). Mean total cost amounted to 10 902 Euros/patient/year (direct medical 67%, direct nonmedical 13%, indirect costs 20%). Drugs, disability pension and informal care were the highest cost items. Costs of mild (Expanded Disability Status Scale 0-3.5) and moderate (Expanded Disability Status Scale 4.0-6.5) disease were 9 218 and 17 634 Euros/patient/year respectively (p<0.01), that is lower than results from Western European countries. Conclusion - Our study provides current inputs for policy making and contributes to understanding variation of costof- illness of multiple sclerosis in Europe.]
[Tissue water content determination based on T1 relaxation time of water and quantitative cerebral 1H MRS at 3T using water as an internal reference]
[Objective - Application of a quantitative MR-spectroscopic method for 3T clinical scanners based on tissue water content as an internal reference. Patients and methods - Six (22±2 yrs) volunteers were involved in the study. We performed T1 relaxation time measurements in a particular slice of the brain at 1T and 3T. Based on the validated water content measurement at 1T, the correlation of relaxation time T1 and water content was determined at 3T. The resulting water content served as internal reference for the quantification of localizated MRspectroscopic measurement. Results - At 3T our method resulted in 37.6±0.5 mol/l and 46.4±1.5 mol/l tissue water content in the white and gray matter, respectively. Calibration based on water content led to following metabolite concentrations: N-acetyl-aspartate 7.79±0.67 mmol/l; creatine 3.76±0.28 mmol/l; choline 3.68±0.47 mmol/l; myo-inositol 10.35±3.70 mmol/l in the white matter; and N-acetyl-aspartate 8.20±0.45 mmol/l; creatine 4.76±0.18 mmol/l; choline 2.64±0.35 mmol/l; myo-inositol 8.32±1.42 mmol/l in the grey matter. Conclusions - Tissue water content based on T1 value at 3T shows good accordance with gravimetric or other MR methods in the literature. Using it as an internal reference resulted in white matter metabolite concentrations that are in the range of previously published data. Comparing metabolite values of grey matter is more difficult because data in the literature substantially differ. The presented method is simple and easily applicable on any MR scanner without complicated correction and calibration steps.]
[Role of the intraoperative electrical brain stimulation in conserving the speech and language function in neurosurgical operations of awake patients]
[Aim of the study - To summarize the results gained with awake craniotomies, which were performed in either low grade glioma patients or epilepsy surgical patients whose tumor or epileptogenic zone, was in the vicinity of eloquent, mostly language, cortices. Patient selection and methods - In our retrospective study we selected 16 patients who were operated awake between 1999-2011 at the Neurosurgical Department of MÁV Kórház Budapest, or at the National Institute of Neurosciences in Budapest, or at the Neurosurgical Department of the University of Debrecen in Debrecen. In the presurgical evaluation if it was possible we performed functional magnetic resonance imaging, tractography and detailed neuropsychological testing. At the National Institute of Neurosciences all patients were operated with the aid of MR guided neuronavigation. Results - Anesthesia was carried out without complications in all of the 16 cases. Monitoring of sleep deepness has significantly contributed to the safety of anesthesia during the superficial anesthezied states of the operation. The intraoperative neuropsychological tasks used for testing language were sensitive enough to judge the little disturbances in speech during stimulation. Stimulation evoked seizures could be adequately managed during surgery and did not influence the outcome of the procedures. The use of neuronavigation helped significantly by planning the optimal place for the craniotomy and by intraoperative orientation. Conclusions - Awake craniotomies require well practiced surgical teams, which requires the cooperation of neuro-anesthesiologits, neurosurgeons, neuropsychologist and electrophysiologists. It has two goals, first to reduce the time of surgery to minimize surgical complications, secondly the detailed intraoperative mapping of cognitive and motor functions to avoid any neurological deficit. The intraoperative anatomical data provided by the neuronavigation and the functional data provided by awake intraoperative stimulation of the patient together serve the safety of the patient which is essential in the neurologically minimal invasive neurosurgical approach of the 21st century.]
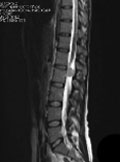
[Multiple sclerosis coexisting with spinal cord ependymoma: a case report]
[Background - In this paper, we report a coexistence of multiple sclerosis and an intradural spinal cord tumor. Case report - A 34-year-old woman who had a history of relapsing-remitting multiple sclerosis for the last 15-years presented with acute sensory loss and spasticity in her left lower limb and her spinal magnetic resonance imaging study revealed an intradural spinal cord tumor in the lumbar spine, further diagnosed as ependymoma. Conclusion - We call attention to this rare association of MS and a spinal cord tumor, emphasizing the need for investigation of new symptoms during the evolution of MS.]
[Developmental neurology, development of the self-awareness, the communication and the movement Marianne Berényi, Ferenc Katona]
[Developmental neurology, development of the self-awareness, the communication and the movement Marianne Berényi, Ferenc Katona 2012;65(09-10)]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.