The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Lege Artis Medicinae - 2021;31(08-09)
Content
[Paradigm shift in the drug therapy of HFrEF]
[The incidence and prevalence of heart failure (HF) is constantly increasing, its morbidity and mortality are still high, thus the disease burden is huge and its proper treatment is of paramount importance. Substantial evidence on improving its prognosis remains available only by the treatment of chronic heart failure with reduced left ventricular function (HFrEF). There have been published a number of “milestone” studies in the last decades, the results of which fundamentally determined the HF therapy until recently. Baseline therapy for HFrEF has been placed on three pillars for a long time: angiotensin-converting-enzyme inhibitors (ACEI), beta-blocker (BB), and mineralocorticoid receptor antagonist (MRA) are included in different heart failure guidelines with I/A level recommendation. The ground-breaking highly important PARADIGM-HF study was published in 2014, and examined an entirely new class of drugs, the sacubitril/valsartan, which belongs to the group of angiotensin receptor blocking/neprilysin inhibitors (ARNI) in HFrEF patients. Results of this study showed that sacubitril/valsartan significantly reduced the primary composite endpoint of CV mortality and HF hospitalization by 20% and reduced overall mortality by 16% compared to an active comparator enalapril, which has the broadest evidence in HFrEF therapy. The 2016 European Society of Cardiology (ESC) HF guidelines recommended the use of sacubitril/valsartan with an I/B evidence level as a replacement for an ACEI to further reducing the risk of HF hospitalization and death of out-patients with HFrEF who remained symptomatic despite optimal treatment with an ACEI, a BB and an MRA. Later, several smaller studies concerned sacubitril/valsartan with slightly different indications and in other patient groups. The PIONEER-HF study demonstrated that early initiation of sacubitril/valsartan therapy after the stabilization of acute HF is safe and effective in HFrEF patients, reduces more rapidly the NT-proBNP levels - which correlates with HF prognosis -, than the enalapril. The TRANSITION and TITRATION studies provided useful information on the initiation of sacubitril/valsartan therapy and the strategy of dose titration. The appearance of sacubitril/valsartan opened a new era in HFrEF therapy a few years ago, an era we are actually experiencing in Hungary. Thanks to SGLT-2 inhibitors, it is also possible that we are at the door of an even newer therapeutic era. This question is expected to be answered in the new ESC HF-guidelines to be published soon this year. ]
[Coronavirus disease-2019 among rheumatic musculoskeletal patients – possible outcomes of infection, severe disease development and effectiveness of vaccination]
[The prevalence of coronavirus infection of patients with inflammatory and rheumatic diseases does not differ significantly from the rate of the disease in the local general population. Patients treated with higher doses of corticosteroids, especially those with more severe systemic autoimmune disease, contract coronavirus infection at a higher rate. The risks of hospitalisation and the mortality rate do not differ significantly from those of the general COVID infected population. Patients treated with high-dose corticosteroids and cytostatic drugs are exceptions of this. Associated diseases that are generally threatening the COVID-19 patients (according to pre-COVID rheumatology surveys) are the same in inflammatory and non-inflammatory rheumatology conditions. Hence, the risk of severe COVID-19 outcome does not essentially depend on rheumatological conditions since the aging itself with typical cardiopulmonary and metabolic diseases are also responsible for. From the treatment armamentarium of inflammatory rheumatology/autoimmune diseases only arbitrarily dosed dexamethasone treatment seems efficacious. In specific patient groups, interleukin 6 antagonists and JAK inhibitors may also have a beneficial effect. The rheumatological and autoimmune drugs as antimetabolites, anti-cytokine immunotherapies and JAK inhibitors, do not increase the risk of COVID-19 infection since it is not necessary to stop them in infected patients. The B-cell antagonist rituximab is the exception since by attenuating humoral immunity and the presence of active disease increase the risk of severe outcome in COVID-19 infected cases. COVID vaccination does not mean specific acute risk for rheumatological and autoimmune patients. The long term effect of COVID vaccination regarding the robustness and sustained immunity specifically in autoimmune and inflammatory diseases needs further studies.]
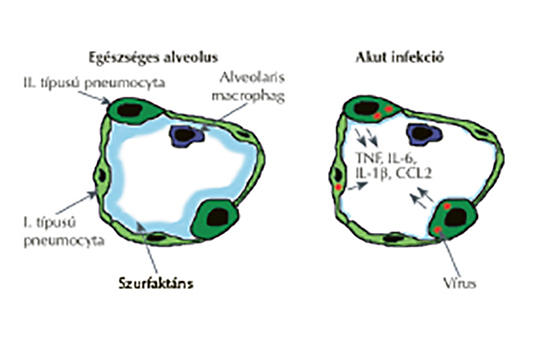
[Pulmonary aspects of COVID-19 infection]
[COVID-19 caused already the most serious pandemic of the past 100 years with increasing morbidity and mortality rates worldwide. Due to the aerosol-born virus, pneumonia develops in a significant part (ca. 20%) of patients with serious forms of acute respiratory distress syndrome (ARDS) ca. in 5-8% of all cases. For patients with chronic obstructive pulmonary disease, it is very important to save their well-controlled condition and to continue the maintenance therapy in co-morbid COVID-19 infection. The role of pulmonary exercises and rehabilitation is crucial. Thus, pulmonology outpatient clinics gained additional follow-up activities such as the long-term post-COVID care with complex functional assessments and regular structural imaging of discharged patients.]
[Manifestations of COVID-19 in pregnancy]
[There are confirmed COVID-19 infections in Hungary since March 2020. This disease caused by SARS-CoV-2 was initially known not to impose special risk on pregnant women, but probably due to the increasing number of cases and the latest mutations, this is no longer true nowadays. Recent outcomes suggest that pregnancy increases the risk of hospital admission, invasive ventilation and death with higher odds of preterm birth and caesarean section. Seemingly, vertical infection occurs only in a small percentage of all cases. To our best knowledge, 7 expectant mothers lost their life in Hungary thus far due to COVID-19. However, further rigorous studies are needed for a more accurate understanding of pregnancy complications.]
[Psychiatric conditions not only influence the severity of clinical outcome of COVID-19 but also the medication of mental diseases]
[The disease process in psychiatric patients who contracted SARS-CoV-2 infection might become more severe because of their impaired general health, comorbidities and unhealthy lifestyle. However, among all psychiatric conditions statistically significant correlation with severe and lethal outcome have been found only in schizophrenia with possible association of multiple immune dysfunctions. While the antipsychotic clozapine used in treatment resistant schizophrenia seems to decrease the likelihood of recovery of patients who underwent COVID-19 infection, antidepressants treatment for major depression may result in more favourable outcome. Mainly the antidepressant fluvoxamine has been reliably found effective by inhibiting cytokine storms observed in some COVID-19 infected patients.]
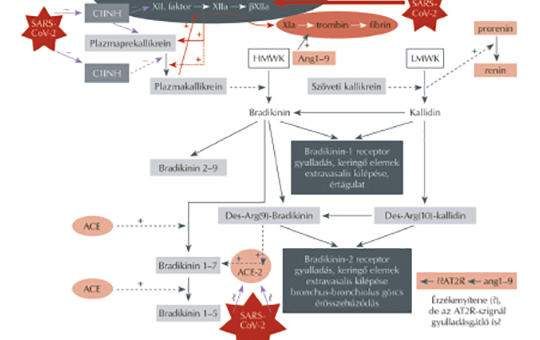
[Bradykinin-cytokin-storm and its pathomechanism in very severe Covid-19]
[The authors review the pathomechanism of severe COVID-19 leading to systemic uncontrollable inflammation, thrombotic events and other complications. The review includes the extremely complex interactions between the infecting coronavirus and the in loco cellular-tissue contact system, the kinin-kallikrein and the renin-angiotensin systems. Authors critically evaluate some potential therapeutic interventions aiming at the mitigation of the dominant bradykinin-cytokine storm in the background of severe COVID-19 by inhibiting bradykinin formation, facilitating its degradation, or blocking either the B2 receptor or the bradykinin induced cytokine response.]
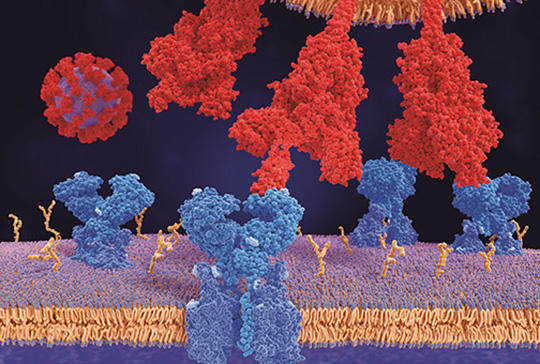
[RAAS inhibitors therapy – COVID-19 pandemic]
[Acute respiratory syndrome with various signs and outcomes caused by the SARS-CoV-2 virus is the biggest challenge facing health systems worldwide today. The renin-angiotensin-aldosterone and kinin-kallikrein systems and within these two endopeptidases (ACE and ACE2) play a crucial role in the developing clinical feature of COVID-19. Adverse effects of the ACE-stimulated Ang II/AT1R axis (oxidant, pro-inflammatory effect, vasoconstriction) are counterbalanced by the ACE2-induced AT2R and MasR activities (antioxidant, anti-inflammatory effect, vasodilation). The severity of SARS-CoV-2 pneumonia and systemic inflammation explains the impairment of ACE2 (as an important defence factor of the lungs) caused by the biding spike protein of the SARS-CoV-2, which decreases the ACE2 levels. In parallel, bradykinin production also increases and intensifies the SARS-CoV-2-induced cytokine storm through the BKB1 and BKB2 receptors. Since the RAAS inhibitors (ACEI, ARB) affect the two regulatory systems and enzymes at different sites and to different degrees, their role must urgently have been clarified in the COVID-19 since their use is essential and general of many population-wide diseases (hypertension, cardiovascular, renal and metabolic conditions). Based on pathophysiological and experimental data, it is reasonable to hypothesize that in COVID-19 with comorbidities, especially in the elderly, the decreased ACE2 expression may be restored by RAAS inhibitors and the missed or reduced protective effect may be revitalised. This protective effect applies to both RAAS inhibitors. Clinical trials clearly support the declared opinion of many international societies that the use of RAAS inhibitors does not increase the risk of the occurrence of SARS-CoV-2 in itself let alone the severe and critical cases. Accordingly, initiated RAAS inhibitor therapy not only may rather must be continued during the development of COVID-19.]
[Possible ophthalmological symptoms and complications of COVID-19 infections]
[The COVID-19 infection that started in December 2019 in China became a pandemic. Initially, the publications were dealing with respiratory symptoms, but later on other non-specific, pandemic related syndromes were discussed in the medical literature, among them more and more ophthalmological symptoms. Essential ophthalmological knowledge is important since the air-born droplet infection is invading generally the mucous membranes. Conjunctiva is the most important mucous membrane of the eyes. Viral particles colonising the conjunctiva reach the nose by the tears and are spreading to the nasopharynx and finally the respiratory system, which is an alternative, ophthalmological way of the invasion. Nevertheless, more researcher doubt this ophthalmic route of the infection. The present study overviews the most important ophthalmological and neuroophthalmological symptoms and syndromes. Intensive care units focus on maintaining the vital functions, however for saved patients there is very important the prevention or early therapy of ophthalmological complications.]
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey3.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries4.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]5.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]1.
Clinical Neuroscience Proceedings
[A Magyar Stroke Társaság XVIII. Kongresszusa és a Magyar Neuroszonológiai Társaság XV. Konferenciája. Absztraktfüzet]2.
3.
Journal of Nursing Theory and Practice
[A selection of the entries submitted to the literary contest "Honorable mission: the joys and challenges of our profession" ]4.
Journal of Nursing Theory and Practice
[End of Life and Palliative Care of Newborns in the Nursing Context]5.
Journal of Nursing Theory and Practice
[Aspects of Occupational Health Nursing for Incurable Patients ]