[Personalized treatment options for spinal muscular atrophy]
SZABÓ-TAYLOR Katalin, MOLNÁR Mária Judit
MARCH 30, 2023
Clinical Neuroscience - 2023;76(3-4)
DOI: https://doi.org/10.18071/isz.76.0077
Review
SZABÓ-TAYLOR Katalin, MOLNÁR Mária Judit
MARCH 30, 2023
Clinical Neuroscience - 2023;76(3-4)
DOI: https://doi.org/10.18071/isz.76.0077
Review
Szöveg nagyítása:
Spinal muscular atrophy (SMA) is an autosomal recessive disease leading to progressive muscle weakness and atrophy, in severe cases also affecting the bulbar and respiratory muscles.The clinical spectrum of the disease is extremely variable, in the most severe cases resulting in perinatal death, while at the least severe end of the spectrum causing some motor deficits in old age without the loss of ambulation. Spinal muscular atrophy care has changed dramatically in recent years due to the availability of new therapeutic options.
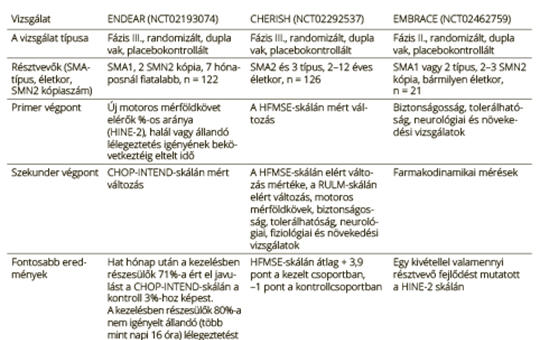
The FDA approved nusinersen in 2016, this was followed by the approval of onasemnogene abeparvovec in 2019 and risdiplam in 2020. The EMA approved all three therapies a year later. Two of the threapies work at the pre-mRNA level, one at the DNA level. The clinical studies leading to the approval of the three drugs included patients of different ages and clinical conditions, and utilised partly different motor and functional scales. Therefore, direct comparison of these clinical studies is not possible. However, an increasing amount of real-world data contribute to the better understanding of the efficacy of the different therapies for patients of different ages and clinical conditions, in a real-world setting. Thus, the question may arise “Which is the best SMA therapy?”. This is an impossible question to answer. Indeed the question “Which therapy is the most suitable for a certain patient at a certain time?” is much more realistic. Here, we provide a brief overview of the objectively measurable results of the three therapies to date and an outlook into future therapeutic avenues.
Clinical Neuroscience
Methanol is a colorless and highly toxic liquid similar to ethanol in odor and taste. Methanol intake can lead to severe metabolic acidosis, loss of vision, permanent neurological damage, and death.
Clinical Neuroscience
Obstructive sleep apnea syndrome (OSAS) may cause daytime sleepiness, mood changes and dysfunction in various cognitive areas due to recurrent arousals and / or chronic intermittent hypoxia. Different possibilities have been proposed regarding the most affected cognitive areas and mechanisms of OSAS. However, it is difficult to compare findings of the different studies due to the fact that individuals with different disease severities were included in the study groups. In the current study, we aimed to determine the relationship between severity of OSAS and cognitive functions, to investigate the effect of continuous positive airway pressure (CPAP) titration treatment on cognitive functions and the relationship between these changes and electrophysiological potential.
The study included 4 groups of patients with simple snoring and mild, moderate and severe OSAS. In the pre-treatment evaluations, verbal fluency, visuospatial memory, attention, executive functions, language abilities and electrophysiological tests for event-related potential were performed. The same procedure was reapplied after 4 months of CPAP-therapy.
Long-term recall scores and total word fluency scores were found to be low in the groups with moderate and severe disease compared to the patients with simple snoring (p: 0.04, p: 0.03, respectively). The information processing time was higher in patients with severe disease compared to patients with simple snoring (p: 0.02). The P200 and N100 latencies related to event related potentials (ERP) were significantly different between the groups (p: 0.004, p: 0.008, respectively). After CPAP treatment, significant differences were found in N100 amplitude and latencies and all cognitive areas except abstraction. In addition, N100 amplitude and latency change rate as well as change in attention and memory abilities were correlated (r: 0.72, p: 0.02; r: 0.57, p: 0.03, respectively).
In the current research, disease severity was found to negatively affect long-term logical memory, sustained attention and verbal fluency. Moreover, significant improvement was detected in all cognitive areas with CPAP treatment. The findings of our study support that changes in N100 potential have the potential to be used as a biomarker that can be used to monitor cognitive function recovery after treatment.
Clinical Neuroscience
To prevent ischemic strokes caused by carotid artery stenosis, carotid artery stenting (CAS) and carotid endarterectomy (CEA) have been utilized. However, complications could be linked to either or both procedures. The purpose of our study is to find the most efficient carotid ultrasound method to forecast periprocedural risk (embolization, new neurological symptoms).
Clinical Neuroscience
To analyze the utility of median nerve (MN) to ulnar nerve (UN) comparative parameters on the diagnosis of carpal tunnel syndrome (CTS) in diabetic patients with distal symmetrical sensorimotor polyneuropathy (DSMPNP).
Clinical Neuroscience
[Drug therapy with non-opioid, opioid and adjuvant drugs is the mainstay of cancer pain relief. The three step analgesic ladder, published by WHO in 1986 Geneva, is useful for oncologists and general practitioners. The first step is giving minor analgesics and adjuvant drugs; the second is giving minor analgesics, weak opioid and adjuvant drugs; the third step is giving minor analgesics, strong opioids and adjuvant drugs.]
Clinical Neuroscience
Stigma is a widespread phenomenon in Parkinson’s disease (PD) and has been shown to affect the quality of life of individuals. This study aims to assess the level of stigma and identify the factors contributing to stigma in patients with PD in Turkey. A total of 142 patients diagno¬sed with PD between June 2022 and March 2023 were included in the study. Sociodemographic data were collected using a sociodemographic information form.
Clinical Neuroscience
Natural disasters, such as earthquakes, frequently result in mood disorders among affected individuals. It is established that neuropathic pain arising from traumatic neuropathies is also linked to mood disorders. This study investigates the influence of neuropathic pain on the development of mood disorders in earthquake survivors with peripheral nerve injuries, following the earthquake centered in Kahramanmaraş on February 6, 2023.
Journal of Nursing Theory and Practice
[The field of healthcare is constantly developing, and the role of nurses is of paramount importance in the optimal care and treatment of patients. Practical education for nurses is essential to acquire the necessary skills and knowledge to provide complex health care to patients. However, traditional hands-on teaching methods are time-consuming and sometimes offer limited opportunities to practice in varied and critical clinical situations.
This article reviews the place and benefits of simulation in the practical education of nurses. The simulation gives nurses the opportunity to practice handling different cases in a realistic, controlled environment, thus improving their decision-making skills and communication skills. After a brief historical overview, it will be presented what types of simulation tools and methods are available for the practical education of nurses and how they support the students’ knowledge acquisition and development.]
Clinical Neuroscience
The aim of this study is to comprehensively determine the types of affected fibers in Parkinson’s disease (PD) patients by employing nerve conduction studies (NCS), sympathetic skin response (SSR) examinations, and current perception threshold (CPT) testing and to analyze the correlation between levodopa use and nerve involvement. This retrospective study included 36 clinically diagnosed PD patients who were recruited between January 2018 and April 2019.
Clinical Neuroscience
Parkinson’s disease (PD) is a heterogeneous neurodegenerative disorder characterized by contradictory clinical outcomes among its several subtypes. The disease can manifest with a tremor-dominant (TD) or a non-tremor-dominant (NTD) phenotype. Although the TD subtype may show a better prognosis, there is limited information on the phenotypic differences regarding the level of axial symptoms. For this reason, in this study it was aimed to make a quantitative comparison of axial posture and spinal mobility between PD with TD and NTD.
Cervical syringomyelia associated with cervical disc disease
A comparison of quantitative parameters of axial posture and spinal mobility between motor subtypes of Parkinson’s disease
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey3.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries4.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]5.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]1.
Clinical Neuroscience Proceedings
[A Magyar Stroke Társaság XVIII. Kongresszusa és a Magyar Neuroszonológiai Társaság XV. Konferenciája. Absztraktfüzet]2.
3.
Journal of Nursing Theory and Practice
[A selection of the entries submitted to the literary contest "Honorable mission: the joys and challenges of our profession" ]4.
Journal of Nursing Theory and Practice
[End of Life and Palliative Care of Newborns in the Nursing Context]5.
Journal of Nursing Theory and Practice
[Aspects of Occupational Health Nursing for Incurable Patients ]