The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Specialities
Endocrinology
Perineural 5% dextrose versus corticosteroid injection in non-surgical carpal tunnel syndrom treatment
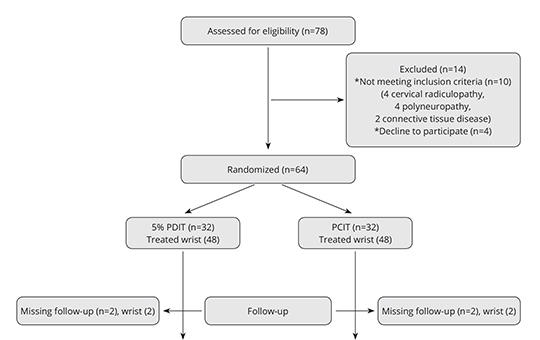
We aimed to investigate the difference of clinical and electrophysiological improvement between perineural corticosteroid injection therapy and perineural 5% dextrose injection therapy in carpal tunnel syndrome. Total of 92 wrists that were diagnosed as mild-to-moderate idiopathic CTS and completed their follow-up were included in our study. The severity of pain, symptom severity and functional status were assessed by visual analog scale.
Lightning strike‑induced cauda equina syndrome: a case report
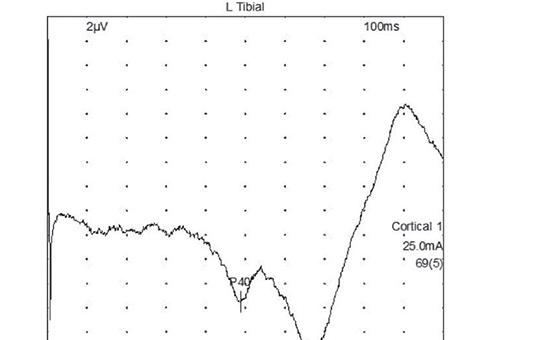
Peripheral nerve injuries after being struck by lightning have been documented. Here, we report a case of cauda equina syndrome induced by lightning. A 27-year-old man presented with numbness, a burning sensation in the saddle region, and increased urinary urgency after being struck by lightning. He had absent Achilles reflexes and paresthesia in the saddle region upon neurological examination, and magnetic resonance imaging of the spine was normal.
[Women and migrain ]
[Migraine is a headache disorder affecting 14% of general population, being even more prevalent (20%) among women in the 20–64 age group, who are actively working and are mainly at reproductive age. 18–25% of migrainous women have an attack related to menstrual cycle, 7% of them having an attack only at this period. Fluctuation of estrogen level may be responsible for these attacks, we can use NSAIDs, slowly acting triptans or progestin-only treatment as short-term prophylaxis. Hormonal contraception is not contraindicated in migraine. Combined (estrogen+progestin) treatment is proposed only in migraine without aura, but in case of more frequent and/or severe attacks or the appearence of an aura treatment should be stopped. In migraineurs with elevated risk of stroke combined hormonal contraception should be used with caution. In migraine with aura patients progestin-only contraception is possible. During pregnancy in 55–91% of migraineus women attacks disappear or are less severe. In most cases migraine with aura attacks occur during this period. Non-pharmacological treatments should be considered as first in the treatment off attacks, with consideration of risk/benefit ratio paracetamol, metamizol or triptans may be used. With the menopause in 2/3 of patients migraine gets better but because of the fluctuation of hormon levels it can be worse than before. Hormonal replacement therapy is not contraindicated in migrainous women but it can result in worsening of migraine. ]
[Nationwide comprehensive health protection screening program in Hungary (2010–2020–2030 – MÁESZ) analysis of blood pressure and metabolic status]
[The “Comprehensive Health Protection Screening Program of Hungary 2010-2020-2030” (MÁESZ) (http://www.egeszsegprogram.eu) is the only complex screening program in Hungary, in which we aimed to map the health status of our country. Between 2010 and 2021, the screening program carried out in the truck was present in 2,406 locations nationwide and performed more than nine million screening tests for more than 280,000 citizens.]
[Patients with diabetes, renal failure and perimenopausal hypertension]
[The determinants of cardiovascular (CV) morbidity and mortality is sympathetic overweight, which is the main risk factor for CVD. factors - hypertension (HT), diabetes mellitus (T2DM), renal function deterioration (CKD), dyslipidaemia and, in women, the perimenopausal status - significantly potentiates the adverse effects of diabetes, dyslipidemia, diabetes mellitus.]
[Important effects of renin-angiotensin system and angiotensin receptor blockers. Focus on valsartan]
[Blockade of AT1-receptors causes arteriolar vasodilation leading to the decrease the total peripheral resistance (TPR), the aldosterone secretion, and the sodium reabsorption in renal tubuli with reduction of the intraglomerular pressure.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.