The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Specialities
Endocrinology
Study protocol of the Hungarian Longitudinal Study of Healthy Brain Aging (HuBA)
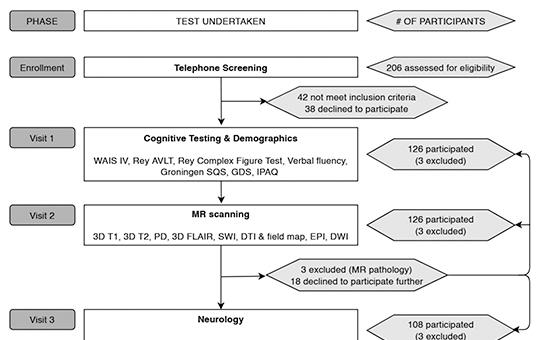
Neurocognitive aging and the associated brain diseases impose a major social and economic burden. Therefore, substantial efforts have been put into revealing the lifestyle, the neurobiological and the genetic underpinnings of healthy neurocognitive aging. However, these studies take place almost exclusively in a limited number of highlydeveloped countries. Thus, it is an important open
Progressive multifocal leukoencephalopathy with a benign prognosis in an immunocompetent patient – A case report
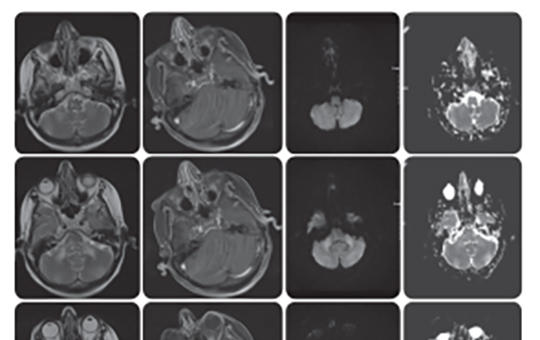
John Cunningham virus (JCV) is most commonly acquired in childhood and is often asymptomatic throughout life. However, in the case of primary or secondary immunosuppression, it is known to cause progressive multifocal leukoencephalopathy (PML) in the central nervous system. Hereby, we describe a rare case of PML in a patient without known factors of immunosuppression or use of immunomodulation.
[Guillain-Barré syndrome caused by intravesical instillation of Bacillus Calmette-Guérin]
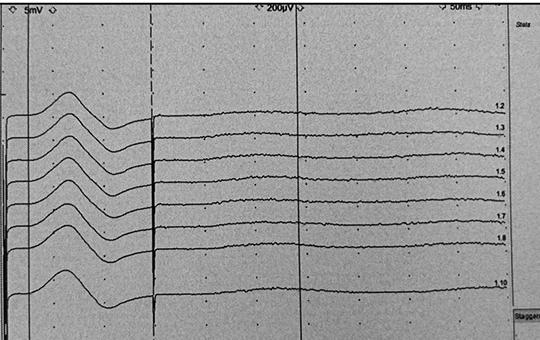
[ Guillain-Barré syndrome is an acute inflammatory demyelinating polyneuropathy. In the vast majority of patients, 1-4 weeks before the onset of GBS-related symptoms, an event such as upper respiratory tract or gastrointestinal tract infection, surgical intervention or vaccination is present. To the best of our knowledge, this is the first case of GBS that occurred after intravesical Bacillus Calmette-Guérin therapy in the absence of tuberculosis or any other infection in the English literature.]
[Recent results of lifestyle and drug-induced body-weight reduction ]
[Among the specific weight loss diets, there is no convincing fundamental difference in their short-term effects. There is no magic bullet since weight regain is common with all methods in the long term (the greater the reduction the greater the regain). Thus for the majority of patients in need none of them has any significant outcome (–10% per 2 years). Only the safety of some dietary methods has been clarified so far. Although the Mediterranean diet is generally accepted (in a broader context, the Smart Plate developed for domestic conditions by the National Association of Hungarian Dietitians too), however intermittent fasting and e.g. the time-restricted eating may also have some advantages. It would be reasonable to attribute more importance to the patient’s preference during the (repeated) dietetic consultations (the question is who could mediate it authentically?) Nutritional therapy requires essentially (or should require) medical treatment of excess weight, which would also support growing-up of obesitology. In metabolic medicine, entero-hormones, primarily glucagon-like peptide-1 receptor agonists (GLP-1 RA), opened a new chapter in the history of medicine. Newer, more effective forms of this drug family make at least 10% weight loss attainable to most of those in need, and as long as their use continues its cardiovascular benefits have also been proven.]
[Reno- and cardioprotective effects of sodium-glucose cotransporter 2 inhibitors beyond treating diabetes mellitus ]
[SGLT2-inhibitors, originally used as antidiabetics, improved unexpectedly the outcome of cardiac diseases (mainly heart failure) and nearly halved the risk of renal events of diabetic patients. More recently, administering these drugs decreased significantly the morbidity and mortality in primary renal endpoint studies and among patients with heart failure – in diabetic and non-diabetic patients respectively. Concerning these recent outcomes and according to international and domestic guidelines, SGLT-2 inhibitors are considered as first line medications in both chronic kidney disease and the whole spectrum of chronic heart failure, and they should be initiated as early as possible in these conditions. Since the beginning of 2024, these drugs which changed significantly the outcome of these diseases can be prescribed with greater support of Hungarian public financing not only for type 2 diabetic patients but non-diabetics too with chronic kidney diseases and heart failure with reduced ejection fraction. ]
[Gynaecological hormone therapy and cardiovascular risk. Part 2: menopausal hormone therapy ]
[Concerning cardiovascular (CV) risk, beside hormonal contraception, menopausal hormone therapy (MHT) has a pre-eminent clinical significance. If women start MHT younger than 60 years of age, or within 10 years after their menopausal transition, the risk of coronary diseases and mortality too decreases. Conventional oral MHT slightly increases the risk of venous thromboembolism (VTE) and stroke, while transdermal admission does not it. MHT initiated in women above 60, raise the risk of cardiovascular (CV) diseases, thus it is useful to start MHT at the onset of menopause syndrome signs (primarily hot flashes), preferably at a younger age. Preventing serious late complications to start and continue MHT at least until natural menopause is essential in premature ovarian insufficiency and early menopause. Below, we summarize the CV implications of MHT and its alternative treatment options.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.