The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Hypertension and nephrology - 2019;23(06)
Content
[Hypertension and brain function. Correlation of high blood pressure and demencia in aging. Hypertension in young-middle adults - demencia in elderly]
[The cerebral vascular damage caused by hypertension is manifested primarily in cognitive dysfunction, which is caused by hypoperfusion of brain tissue, ischemic, or bleeding stroke, or white matte injury. Hypertension may not only result in cerebral damage to the vascular background - dementia -, but may also contribute to the development and progression of classical gene-related Alzheimer’s disease. Blood pressure gradually increases in the elderly and in the very elderly, and the frequency of hypertension-mostly as isolated systolic hypertension - is 50% to 70%. High blood pressure predominately, or in full, means not only an increase in the circulatory resistance of the small children, but also, as part of the aging of the body, the rigidity (stiffness) of the arteries. At the same time, the incidence of dementia, along with age, rises sharply - up to 20% in those over 65 years of age, and over 40% in 80-90 years of age. The relationship between high blood pressure and dementia from the young age to the very old age may change as a function of current age. In the very old age of life, the varying influence of other pathological factors other than hypertension is becoming more and more important in the deterioration of both the vascular structure and the brain function. In this late stage of life, the very advanced rate of aging and nutritive blood flow often require higher perfusion pressure, and the not enough thought-out blood pressure reduction can be more damaging than a protective effect on brain condition or function. SPRINT MIND - the Intense Blood Pressure Reduction - hasn’t resolved the question, and we can legally assume that the 130-140 Hgmm SBP. Is the most favorable for dementia. The value of DBP 70 Hgmm is definitely unfavorable.]
[Predictive factors for ischemic heart disease, diabetes mellitus and chronic kidney disease among hypertensive patients based on the data of the Hungarian Hypertension Registry 2011-2013-2015. Part I. Hypertensive population aged 35 to 64 years]
[The association of hypertension with ischemic heart disease, diabetes and chronic kidney disease is the greatest therapeutic challenge because these associations significantly increase mortality and deteriorate life expectancy. It is important for the clinician to clarify the predictive factors of each association for successful prevention or slowing the progression of diseases. According to the database of the Hungarian Hypertension Registry 2011-2013-2015, 11,137 men and 11,112 women with hypertension and comorbidities (CHD, diabetes, CKD) aged between 35 and 64 were analyzed for the purpose of assessing the predictive value of the traditional risk factors in co-morbidity. We analyzed the predictive weight of each variable with single- and multi-variable stepwise logistic regression, and reported Odds ratio (OR, odds ratio). In patients with hypertension aged 35-64 (male / female), the prevalence of CHD was 41.6% / 35.8%, diabetes 27.1% / 23% and KVB 16.2% / 33.8%, respectively. The chance of developing CHD is highest in hypertensive individuals (male/female) who have diabetes (OR 1.30/1.48), who are obese (OR 1.22/1.21), who smoke (OR 1.50/1.51), and whose blood pressure >140/90 mmHg (OR 1.23/1.29). The dominant predictive factors of type 2 diabetes are obesity (visceral obesity) (OR 1.46/1.49), low HDL cholesterol (OR 1.32/1.35), and high triglyceride levels (OR 1.20/1.42); in women the uric acid level also showed high odds ratio (OR 1.39). There is a significant chance of developing chronic kidney disease in hypertension in both sexes, if abnormal uric acid levels (OR 1.73/1.46) and inadequate treatment of high blood pressure (>140Hgmm SBP) (OR 1.43/1.19) are present. In women, the abnormal triglyceride level) also showed a high odd (OR 1.81).]
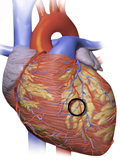
[Serotoninergic drugs for weight loss. A review of efficacy and cardiovascular safety of lorcaserin]
[Complex therapy of obesity consist the medical treatment. Several weight lowering drugs are available in the United States, one of which is 5-HT2c agonist lorcaserin. After failures with former non-selective serotoninergic agents (fenfluramine, dexfenfluramine), there was great anticipation and more questions about the release of lorcaserin, which proved its effectiveness and safety in several phase 3 studies. Lorcaserin is a selective agonist of 5-HT2c receptors, therefore free form adverse effects of former non-selective serotoninergic drugs on valvulopathy or pulmonary hypertension. The results of the recently published CAMELLIATIMI 61 study confirmed the cardiovascular safety of lorcaserin.]
[The effect of the β-blockers on left ventricular sytolic and diastolic function]
[The author surveys the pharmacodynamic effects, by which the β- blockers can exercise an influence on systolic and diastolic function. He points out, that the constituents of the effect can be separated only in didactic aspect, its worthwile to take the situation of their interdependence. Analyses the how the when and the wherefore the hemodynamic state determines the component of the complex mode of action that sets off. Deals with the problem, that what kind of effects are desired in certain clinical settings and which of those are deletorious. On emphasized he discusses the greatest danger of the β-blockade, the negative inotropic effect, and the mode of its offset or rather counteraction of its hemodinamic result.]
1.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?2.
Clinical Neuroscience
Neuropathic pain and mood disorders in earthquake survivors with peripheral nerve injuries3.
Journal of Nursing Theory and Practice
[Correlations of Sarcopenia, Frailty, Falls and Social Isolation – A Literature Review in the Light of Swedish Statistics]4.
Clinical Neuroscience
[Comparison of pain intensity measurements among patients with low-back pain]5.
Journal of Nursing Theory and Practice
[Fear of Falling among Geriatric Patients: a Narrative Review]1.
2.
3.
4.
5.