The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Hypertension and nephrology - 2019;23(05)
Content
[The importance of brain-derived neurotrophic factor in psychopathology and cardiovascular conditions: psychosomatic connections]
[Cardiovascular diseases and mood disorders are common public health problems worldwide. Their connections are widely studied, and the role of neurotrophins, especially brain derived neurotrophic factor (BDNF) is already supposed in both conditions. However, no reviews are available describing possible associations between cardiovascular risk and mood disorders based on BDNF. Decreased level of BDNF is observed in depression and its connection to hypertension has also been demonstrated with affecting the arterial baroreceptors, reninangiotensin system and endothelial nitric oxide synthase activity. BDNF was also found to be the predictor of cardiovascular outcome in different patient populations. Our aim was to overview the present knowledge in this area demonstrating a new aspect of the associations between mood disorders and cardiovascular diseases through the mediation of BDNF. These findings might enlighten a new psychosomatic connection and suggest a new therapeutic target that is beneficial both in respect of mood disorders and cardiovascular pathology.]
[Non-invasive evaluation of cardiovascular risk in pediatric chronic kidney disease patients]
[Cardiovascular diseases are the leading cause of mortality and morbidity in children with chronic kidney disease (CKD). Similar to adults, children with CKD experience a high burden of traditional and uremia-associated risk factors. Recent years, several studies were published in connection with cardiovascular risk factors, patomechanism, and early markers of cardiovascular diseases. Early signs of cardiomyopathy, such as left ventricular hypertrophy or dysfunction, and markers of atherosclerosis, such as increased intima-media thickness of the carotid artery or increased wall stiffness of the aorta are frequently present in early stages of CKD in children. As prevention is important in pediatrics, the evaluation of subtle changes of the cardiovascular system provide opportunity for early treatment and that enables children to develop normally and have a better long-term quality of life. Recently, newer non-invasive cardiovascular imaging modalities have been emerged to diagnose subclinical alterations of the heart and vessels in this specific population with kidney disease. In this review, we provide an overwiev of the emerging imaging techniques used to detect early subclinical organ damage in pediatric chronic kidney disease patients.]
[GLP-1 receptor agonists in the treatment of type 2 diabetes]
[The glucagon-like peptide (GLP)-1 receptor agonists and somewhat later, the sodium-glucose cotransporter (SGLT) -2 inhibitors have brought new perspectives in the antihyperglycemic treatment of type 2 diabetes. The article overviews clinicopharmacologic characteristics of the GLP-1 receptor agonist group, their glycemic and non-glycemic effects, results of the cardiovascular endpoint studies as well as their place in the recent therapeutic guidelines. It is proven, that both glycemic and weight reducing effect is greater of the long-acting (non-prandial) coumpounds as compared to that of the short acting (prandial) derivates, further, that in studies with cardiovascular endpoints they reduced the relative risk of the composite endpoint of non-fatal myocardial infarct, non-fatal stroke and cardiovascular death. Due to the favolurable glycemic and non-glycemic properties their use is advised already in the early course of type 2 diabetes, as combination of the metformin therapy.]
[Blood pressure management for stroke prevention and in the acute stroke. The new guideline of European Society of Hypertension (ESH, 2018), European Society of Cardiology and Hungarian Society of Hypertension (HSH, 2018)]
[Hypertension is the leading modifiable risk factor for stroke. Its prevalence amongst stroke patient is about 60-70% and the benefit of blood pressure (BP) lowering therapy on stroke risk reduction is well established. However the optimal BP targets for preventing stroke and reducing stroke consequences have been controversial. The new European (ESC/ESH) and Hungarian (HSH) hypertension guideline published in 2018 highlighted the primary and secondary prevention of stroke and the BP management in the acute stroke care as well. According results from ACCORD, SPRINT, HOPE-3, and other metaanalysis the systolic blood pressure (SBP) lowering < 120 mmHg has not favourable effect, thus in hypertensive patients < 65 years the SBP should be lowered to a BP range of 120-129 mmHg. In older patients ≥ 65 years the SBP should be targeted to a BP range of 130-139 mmHg (IA). In patients with acute intracerebral haemorrhage careful acute BP lowering with iv. therapy, to <180 mmHg should be considered only in case of SBP ≥ 220 mmHg (IIaB). In patients with acute ischaemic stroke who are eligible for iv. thrombolysis, BP should be carefully lowered and maintained to < 180/105 mmHg for at least the first 24 h after thrombolysis (IIaB). If the patient is not eli gible for lysis and BP ≤ 220/110 mmHg, routine BP lowering drug therapy is not recommended inside 48-72 h (IA). In patients with markedly elevated BP > 220/110 mmHg who do not receive fibrinolysis, drug therapy may be considered, based on clinical judgement, to reduce BP by 15% during the first 24 h after the stroke onset (IIbC). After 72 h of acute stroke in case of hypertensive patients < 65 years the SBP should be lowered to a BP range of 120-129 mmHg (IIaB). In older patients ≥ 65 years the SBP should be targeted to a BP range of 130-139 mmHg (IA). If BP < 140/90 mmHg after stroke, the BP lowering should be considered (IIbA). It is recommended to initiate an antihypertensive treatment with combination, preferably single pill combination of renin-angiotensin system blockers plus a calcium channel blocker and/or a thiazide like diuretics (IA). Lowering SBP < 120 mmHg is not recommended due to advers events regardless of age and type of stroke either in primary or secondary stroke prevention.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
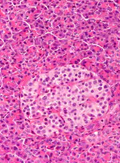
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.