The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2021;74(11-12)
Content
[Relationships between COVID-19 disease, nutritional status, and dysphagia, particularly in stroke patients ]
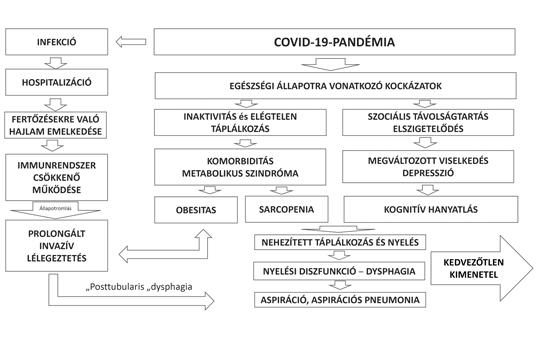
[The new coronavirus, SARS-CoV-2, which causes the COVID-19 disease can lead to severe acute respiratory distress syndrome (ARDS). It poses a serious challenge to the health care system, especially intensive care. Neurological patients, usually of advanced age and with a myriad of comorbidities, are at particular risk through the impact of the new coronavirus on their condition and nutritional capacity. Stroke is a leader in morbidity and mortality data, with a focus on dysphagia and its complications due to COVID-19 disease and acute cerebrovascular accident. In the acute phase of stroke, 30-50% of patients suffer from dysphagia, which still shows a prevalence of 10% six months later. Dysphagia results in decreased or insufficient fluid and nutrient uptake, supplemented by inactivity, leading to malnutrition and sarcopenia, which worsens overall condition, outcome, and rehabilitation efficiency. Screening and early detection of swallowing disorders is a fundamental issue in order to develop a personalized and timely-initiated nutritional therapy strategy. Nutritional therapy plays a key role in frequent intensive care due to COVID-19 disease, where it increases the chances of recovery and reduces the length of stay in the intensive care unit and mortality. This is especially true in critically ill patients requiring prolonged ventilation. In COVID-19 diagnosed patients, screening for dysphagia, bedside assessment, and instrumental examination, followed by swallowing rehabilitation, are of paramount importance. Stroke can also be a complication of the COVID-19 infection. Care for cerebrovascular patients has also adapted to the pandemic, “triazination” has become systemic, and dysphagia screening for stroke patients and nutritional therapy adapted to it have also shed new light. ]
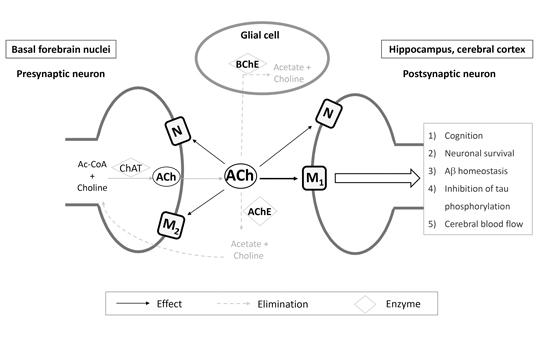
Cholinesterase inhibitors and memantine for the treatment of Alzheimer and non-Alzheimer dementias
In aging societies, the morbidity and mortality of dementia is increasing at a significant rate, thereby imposing burden on healthcare, economy and the society as well. Patients’ and caregivers’ quality of life and life expectancy are greatly determined by the early diagnosis and the initiation of available symptomatic treatments. Cholinesterase inhibitors and memantine have been the cornerstones of Alzheimer’s therapy for approximately two decades and over the years, more and more experience has been gained on their use in non-Alzheimer’s dementias too. The aim of our work was to provide a comprehensive summary about the use of cholinesterase inhibitors and memantine for the treatment of Alzheimer’s and non-Alzheimers’s dementias.
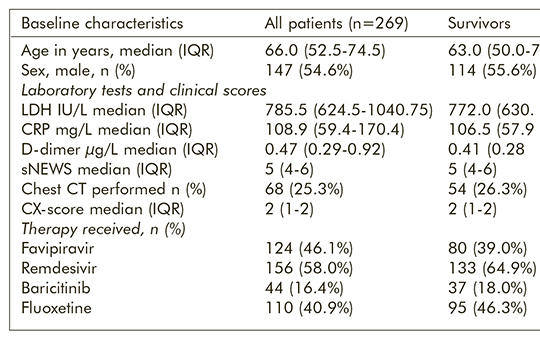
Fluoxetine use is associated with improved survival of patients with COVID-19 pneumonia: A retrospective case-control study
We aimed to investigate the association between fluoxetine use and the survival of hospitalised coronavirus disease (COVID-19) pneumonia patients. This retrospective case-control study used data extracted from the medical records of adult patients hospitalised with moderate or severe COVID-19 pneumonia at the Uzsoki Teaching Hospital of the Semmelweis University in Budapest, Hungary between 17 March and 22 April 2021. As a part of standard medical treatment, patients received anti-COVID-19 therapies as favipiravir, remdesivir, baricitinib or a combination of these drugs; and 110 of them received 20 mg fluoxetine capsules once daily as an adjuvant medication. Multivariable logistic regression was used to evaluate the association between fluoxetine use and mortality. For excluding a fluoxetine-selection bias potentially influencing our results, we compared baseline prognostic markers in the two groups treated versus not treated with fluoxetine. Out of the 269 participants, 205 (76.2%) survived and 64 (23.8%) died between days 2 and 28 after hospitalisation. Greater age (OR [95% CI] 1.08 [1.05–1.11], p<0.001), radiographic severity based on chest X-ray (OR [95% CI] 2.03 [1.27–3.25], p=0.003) and higher score of shortened National Early Warning Score (sNEWS) (OR [95% CI] 1.20 [1.01-1.43], p=0.04) were associated with higher mortality. Fluoxetine use was associated with an important (70%) decrease of mortality (OR [95% CI] 0.33 [0.16–0.68], p=0.002) compared to the non-fluoxetine group. Age, gender, LDH, CRP, and D-dimer levels, sNEWS, Chest X-ray score did not show statistical difference between the fluoxetine and non-fluoxetine groups supporting the reliability of our finding. Provisional to confirmation in randomised controlled studies, fluoxetine may be a potent treatment increasing the survival for COVID-19 pneumonia.
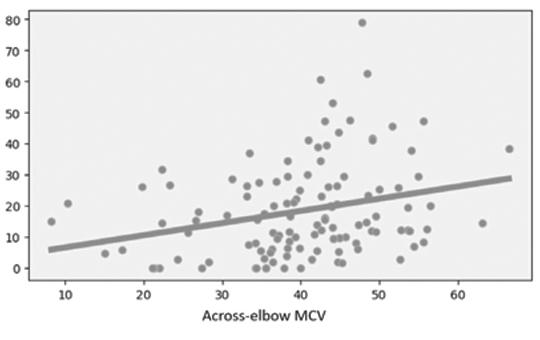
Diagnostic values of conventional conduction parameters in ulnar neuropathy at elbow
Conventional parameters used in electrodiagnosis of ulnar neuropathy at elbow (UNE) are: (i) absolute across-elbow ulnar nerve motor conduction velocity (MCV), (ii) reduction rate of composed muscle action potential (CMAP) amplitude from above to below elbow stimulation, and (iii) MCV difference between forearm and across-elbow segment. We aimed to search the diagnostic accuracy values of these parameters on UNE, and their correlations with axonal dysfunction of ulnar nerve fibers. Arms with clinical signs of UNE and two-fold healthy controls were included. We detected the best cut off points of the measured parameters and their possible combinations. Their diagnostic accuracy values and correlations with parameters reflecting the axonal functions were analyzed, statistically. Totally, 118 arms with UNE and 236 controls were included. Absolute across-elbow MCV yielded a higher accuracy than MCV difference and reduction rate of CMAP amplitude (p = 0.010 and p˂0.001, respectively). Besides, combining it with other parameters did not increase the diagnostic yield. Correlation analyses revealed that the only parameter having positive linear correlations with sensory nerve action potential amplitudes both in the control and the disease groups is the absolute across-elbow MCV. The absolute across-elbow MCVs have also positive linear correlation with CMAP amplitudes in disease group. The absolute across-elbow MCV is the most valuable conventional parameter for the electrodiagnosis of UNE. It is also the most correlated parameter with the electrodiagnostic parameters reflecting the axonal functions of the ulnar nerve fibers.
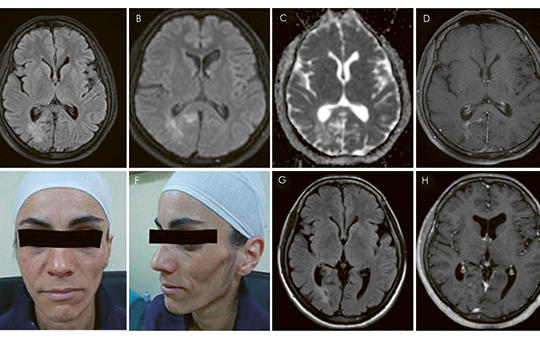
Parry-Romberg syndrome: is it a “relapsing-remitting” disease?
Parry-Romberg syndrome, also known as progressive hemifacial atrophy, is a rare, slowly progressive disorder characterized by unilateral, painless atrophy of the skin and subcutaneous tissue of the face. Neurological manifestations such as epilepsy, migraine and trigeminal neuralgia are relatively common and accompany in 15-20% of cases. Various etiologies such as infection, trauma, embryonic developmental dysfunction, sympathetic dysfunction and autoimmune disorders have been suggested as possible causes. Here we describe a 37-year-old woman whose disease manifested with dynamic contrast enhanced white matter changes over a period of two years, suggesting a “relapsing-remitting” course. Besides the inflammatory activity, positive serum-autoantibodies, inflammatory findings in cerebrospinal fluid, and an overlapping systemic autoimmune disorder may further support the hypothesis of autoimmune-inflammatory mediated pathogenesis.
[Effective therapy in highly active pediatric multiple sclerosis ]
[Multiple sclerosis (MS) is typically a disease of young adults. Childhood MS can be defined in patients under 18 years of age, although some authors set the limit under the age of 16 formerly known as “early-onset multiple sclerosis” or “juvenile multiple sclerosis”, seen in 3-5% of all MS patients. Nowadays, owing to ever-evolving, better diagnostic tools and well-traced, strictly defined diagnostic criteria, childhood MS is showing an increasing incidence worldwide (0.05-2.85/100 000). MS is characterized by recurrent episodes of the central nervous system with demyelination separated in space and time. In childhood almost exclusively the relapsing-remitting (RR) type of MS occurs. Based on experience in adults, the goal in the pediatric population is also the early diagnosis, to initiate adequate DMT as soon as possible and to achieve symptom relief and good quality of life. Based on efficacy and safety studies in the adult population, interferon β-1a and glatiramer acetate were first approved by the FDA and EMA for the treatment of childhood MS also. The increased relapse rate and rapid progression of childhood MS and unfavorable therapeutic response to nearly 45% of the first DMT necessitated the testing of more effective and second-line drugs in the population under 18 years of age (PARADIGMS, CONNECT). Although natalizumab was reported to be effective and well-tolerated in highly active RRMS in childhood, evidence based studies were not yet available when our patients’ treatment started. In this article, we report on the successful treatment of three active RRMS patients with individually authorized off-label use of natalizumab.]
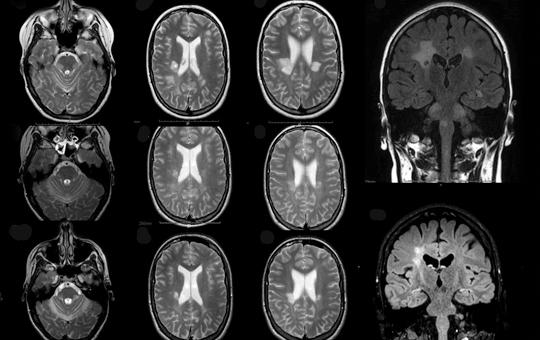
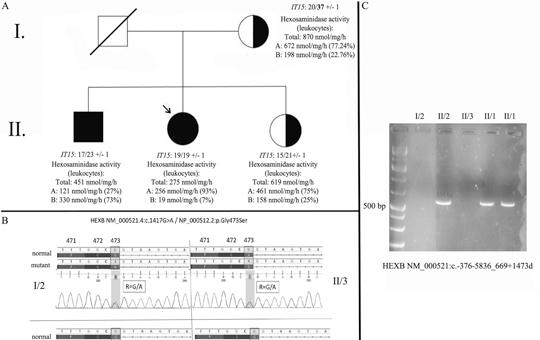
Atypical presentation of late-onset Sandhoff disease: a case report
Sandhoff disease is a rare type of hereditary (autosomal recessive) GM2-gangliosidosis, which is caused by mutation of the HEXB gene. Disruption of the β subunit of the hexosaminidase (Hex) enzyme affects the function of both the Hex-A and Hex-B isoforms. The severity and the age of onset of the disease (infantile or classic; juvenile; adult) depends on the residual activity of the enzyme. The late-onset form is characterized by diverse symptomatology, comprising motor neuron disease, ataxia, tremor, dystonia, psychiatric symptoms and neuropathy. A 36-year-old female patient has been presenting progressive, symmetrical lower limb weakness for 9 years. Detailed neurological examination revealed mild symmetrical weakness in the hip flexors without the involvement of other muscle groups. The patellar reflex was decreased on both sides. Laboratory tests showed no relevant alteration and routine electroencephalography and brain MRI were normal. Nerve conduction studies and electromyography revealed alterations corresponding to sensory neuropathy. Muscle biopsy demonstrated signs of mild neurogenic lesion. Her younger brother (32-year-old) was observed with similar symptoms. Detailed genetic study detected a known pathogenic missense mutation and a 15,088 base pair long known pathogenic deletion in the HEXB gene (NM_000521.4:c.1417G>A; NM_000521:c.-376-5836_669+1473del; double heterozygous state). Segregation analysis and hexosaminidase enzyme assay of the family further confirmed the diagnosis of late-onset Sandhoff disease. The purpose of this case report is to draw attention to the significance of late-onset Sandhoff disease amongst disorders presenting with proximal predominant symmetric lower limb muscle weakness in adulthood.
Rare complication of West Nile viral encephalitis
In our case report, we are presenting a 72 years old male patient. The patient’s symptoms were fever, dizziness, general weakness at the time of admission. The laboratory and CSF tests revealed central nervous system inflammation. West Nile virus was identified from the cerebrospinal fluid. After the symptoms of infection and during supporting treatment, severe, progressing hyponatremia evolved with unknown pathology. According to previous investigations and our diagnostic and therapeutic algorithm cerebral salt wasting syndrome identified as occasion.
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.