The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2011;64(11-12)
Content
[Theoretical and practical considerations of rational polytherapy in epilepsy]
[Author analyses the consideration of rational polytherapy for epilepsy. Among the theoretical aspects he points the different effect of seizure inhibitory drugs on the epilepsy models but didn’t find data enough for the basis of any successful combination. Combinations of compounds having different way of action are more promising. Rational polytherapy can serve also the epileptic patients’ tailored therapy in the daily routine. There have already been some proved synergisms concerning drug interactions. Based on detailed analysis of side effects a possibility occurs for neutralization of side effects when anticonvulsants with side effects of opposite nature are combined. Considering both the side effect profiles and the different (somatic and psychic) habits of the patients we can create a special list of favourable combinations. Co-morbid states and their treatments play a significant role in the application of rational polytherapy. Combination of anticonvulsants of lower potential but without drug-interactions can be the choice in these cases. The non-epileptic indications of the anticonvulsants can also be utilized in polymorbid patients. Based on the theoretical and practical considerations the author defines the ten-step-cognitive-preparation-process in planning the optimal (poly)therapy. On speculative basis he suggests eight beneficial versions of seizure inhibitory rational polytherapy.]
[The carrier model of neurology in Hungary: a proposal for the solution until 2020]
[Based on our previous survey on the capacities of neurological services and on the predictable changes in the neurologist workforce in Hungary, we present a proposal for the organization of the structure of neurological services in the future. We discuss the diagnostic groups treated by neurologists, the neurological services and their progressive organization. Using the current capacities as baseline, we propose patient groups to be treated by neurologists in the future, and the levels of services. Based on the tendencies seen in the last years we suggest to consider to allocate acute stroke services exclusively to stroke units in neurological departments, and we identify a few other diagnostic groups where neurology should have a larger share in patient care. We define three levels for inpatient care: university departments, regional/county hospitals, city hospitals. Instead of minimum criteria we assign outpatient and inpatient standards that are functional from the economic point of view as well. University departments cover all areas of neurological services, have a function in graduate and postgraduate training, and on a regional basis they participate in professional quality assurance activities at the county and city hospital levels, and would have a more independent role in residency training. As far as patient care is concerned, the task of the regional/county hospitals would be similar to that of university departments - without the exclusively university functions. A general neurological service would be offered at the city hospital level - the representation of all subspecialties of neurology is not required. Neurorehabilitation would be organized at special units of neurological wards at the city hospital level, at independent neurorehabilitation wards in regional/county hospitals, and also as an outpatient service offered at the patients’ home. The most significant organizational change would affect the outpatient neurological services. In addition to the special outpatient units associated with university departments and regional/county hospitals, the general neurological outpatient services would be organized as private practices, similarly to the current system of general practitioners, where the individual practices contract independently with the health insurance fund. Their task would be a general neurological service offered 30 hours per week, and also basic, screening neurophysiological and neurosonological examinations, with proper equipment and trained assistance. A transformation in residency training and a change in financing is needed for this plan to fulfill.]
[Vascular or “lower body parkinsonism”. Rise and fall of one diagnosis]
[The “arteriosclerotic parkinsonism”, which is called vascular parkinsonism (VP), was first described by Critchley1. The broad based slow gait, reduced stride lenght, start hesitation, freezing and paratonia was mentioned as “lower body parkinsonism” (LBP) which can be associated by slow speech, dysexecutive syndrome, and hand tremor of predominantly postural character. In VP the DAT-scan proved normal dopamine content of the striatum in contrast with Parkinson’s disease (PD). Additionally, Lewy bodies of brainstem type were not found in VP. Probability of VP increases if central type pathologic gait is prominent; the hands are slightly involved, the MRI indicates transparent periventricular white substance and/or brain atrophy. In some cases differentiation of gait apraxia and parkinsonism could be challenging. There is no rigor of the lower limbs at rest in neither of them, the disturbance of movement is evoked by the gait itself. Three subtypes of “gait ignition failure” has been recently described: (1) ignition apraxia, (2) equilibrium apraxia and (3) mixed gait apraxia. The primary progressive freesing gait was considered as a Parkinson-plus syndrome. Freesing occurs more frequently in diseases with pakinsonism than in PD. The grade of ventricle dilatation and the frontal leukoaraiosis was similar in LBP and gait apraxia. In cases of normal pressure hydrocephalus the impaired gait may mimic PD. Pathologic gait in VP can be explained by the lesions of the senso-motor association pathways in dorsal paramedian white substance within the vulnerable borderzone region. These may be colocalized with the representation of the lower extremities in the posterior third of the supplementer motor area. Rektor2 proposed to change the name of LBP to “cerebrovascular gait disorder”. Notwithstandig central type gait disorder develops also in many degenerative diseases other than cerebro-vascular origin. The neuronal net controling the regulation of movement is widespread, therefore several cortical and subcortical lesions could elicit large variations of pathologic gait, ie.: ataxia, apraxia, ignition failure, akinesis etc. In conclusion: most of the central gait disorders regarding the pathology and their appearance can not be called “parkinsonism”; these are much closer related to the localization of lesions rather than to the diagnostic categories.]
[Subarachnoid hemorrhage in Hungary. Analysis based on the reports of the hospitals to the National Health Insurance Fund in 2009]
[Background and purpose - We analyzed the statistical characteristics of subarachnoid hemorrhage (SAH) in Hungary in 2009. Methods - Using data supplied by the hospitals about their inpatient services to the National Health Insurance Fund with ICD-10 code I60. Results - 1403 SAH hospital cases were recorded in 1028 patients. That is much more than we expected from previous data. 63.6% were women, hospital case fatality was 12.2%. The average hospital stay was 6.47 days. 763 CT examinations were done (74.2% of the patients). Hypertension was recorded in 61.3% of the patients. The incidence was increasing with age till the age group of 51- 60 years, and decreased beyond that. In 531 patients the source of bleeding could be verified. Aneurysm of the anterior communicating artery was more frequent in men, aneurysm of the middle cerebral artery (MCA) and internal carotid artery in women. In total MCA aneurysm was the most frequent. Arteriovenous malformation was present in 7.6% of the patients. SAH was most frequent in January and February, rarest in April and August. Conclusion - SAH is more frequent in Hungary than previously thought.]
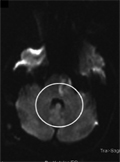
[A8344G mutation of the mitochondrial DNA with typical mitochondrial encephalomyopathy with lactic acidosis and stroke like episodes syndrome]
[We report an unusual case of juvenile ischaemic stroke syndrome associated with the A8344G mutation in tRNALys gene of mitochondrial DNA. The clinical phenotype of patient was typical for MELAS (mitochondrial ecephalomyopathy with lactate acidosis and stroke like episodes). The MELAS has been related to mutation A3243G in most cases, but some other mitochondrial DNA mutations were described in the background of this syndrome as well. A 22-years-old man and his family were investigated. Throughout clinical investigation as well as Doppler sonography, neuroradiological, and immunserological examinations were performed. Molecular studies included the analysis of the Leiden, prothrombin G20210A and the most common mitochondrial DNA mutations. The DNA analysis of the proband revealed a heteroplasmic A8344G substitution in the T-loop of the tRNALys gene. The mutation could not been detected in her mother blood. We can conclude that A8344G mutation of the mitochondrial DNA resulted in juvenile ischemic stroke, which is associated only rarely to this genetic alteration. In young age onset of a stroke-like episode with undetermined etiology the mtDNA alterations always have to be excluded.]
[Common variable immunodeficiency with coexisting central nervous system sarcoidosis. Case report and literature review with implications for diagnosis and pathogenesis]
[We describe a patient with a history of longstanding primary generalised epilepsy, on anticonvulsant therapy, who presented with fever, headache, worsening seizures and hallucinations. Among various investigations, the patient had high CSF protein and ACE levels, leptomeningeal nodular enhancement on MRI brain and non-caseating granulomas in the brain and meninges on the biopsy. The patient was diagnosed with neurosarcoidosis. Subsequently, he was found to be panhypogammaglobulinaemic and was diagnosed with probable common variable immunodeficiency (CVID). The coexistence of common variable immunodeficiency and neurosarcoidosis is rare. Typically, non-caseating granulomas in CVID patients are localised in the lymphatic tissue and solid organs. To our knowledge, there are only five reports of the granulomas of the central nervous system (CNS) in CVID. We discuss the diagnostic difficulties in this case and review the literature.]
[Complementer medicine - on principles of evidence based medicine]
[Complementer medicine - on principles of evidence based medicine 2011;64(11-12)]
[Account on the scientific meeting of Környey Society in 2011. Part 1.]
[Account on the scientific meeting of Környey Society in 2011. Part 1. 2011;64(11-12)]
[Account on the XIXth Congress of Hungarian Neuroradiological Society]
[Account on the XIXth Congress of Hungarian Neuroradiological Society 2011;64(11-12)]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.