The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2011;64(05-06)
Content
[Excerpts of achievements of pharmaceutical cerebro-vascular protection, with especial regard to the statins]
[Despite that hypercholesterinemia is not a risk factor of stroke, treatment with statins is able to reduce these events in a clinically relevant degree. Intervention trials suggest that while for primary prevention, statins are effective in conventional dose, after stroke or TIA this is true only if LDL-cholesterol is reduced below 1,8 mmol/L. To reach this goal, usually intensive antilipid treatment is necessary. There are studies showing beneficial impacts of other lipid drugs, beyond statins, i.e. fibrates and fish oil (among the settings of primary, and secondary preventions, respectively). Against cerebro-vascular events, pleitropic effects of some antihypertensive and antidiabetic medications can also be established.]
[The role of sleep dynamics and delta homeostasis in cognitive functions]
[The paper is aimed to introduce the neuronal network basis of dynamic sleep processes, including the micro-structure of sleep and the relationship of sleep dynamics with homeostatic regulation and plastic changes during sleep. Newer studies tend to show that beyond the wellknown long-term homeostatic and circadian regulation of NREM sleep, sleep is regulated by a stimulus and arousal dependent flexible defense system, the elements of which participate in sleep delta homeostasis. Within the EEG elements of sleep a more larger amount represents reactible type as it was thought previously.. Both the events of wake state and sensory input during sleep are shaping the sleep EEG in a function- and localisation specific way and the next day cognitive functios are determined by these changes.]
[Neurology 2009: a survey of the neurological capacities, their utilization and neurologists based on the 2009 reports of the institutions in Hungary]
[A detailed information on the quantitative and qualitative features and the regional distribution of the current neurological services at the national level is necessary for the planning of health care provision for the future. We present the characteristics of the current neurological services analyzing the database of the National Health Insurance Fund for 2009. This database is exceptionally large and detailed compared to similar data sources in Europe. We examine the number of patients and cases treated both in hospitals and at outpatient units, and also present the distribution of major diagnoses based on ICD-10. We discuss the major problems in three groups: the decrease of capacities; the fragmentation of capacities; and the uneven distribution of workload on neurologists. Number of neurological hospital beds, weekly hours of neurological outpatient capacity, and the number of neurologists are presented. In the analysis of the utilization of capacities we give the number of patients, the number of cases and the financing of the professional performance. We characterize the workload of neurologists by the mean daily number of patients seen by a neurologist, by the number of outpatient units served by one neurologist during the year, and by the proportion of the total workload on each neurologist. Neurological capacities significantly decreased in the period of 2004-2009: 12 hospital neurological wards were closed, and with further decreases in bed numbers the original 3733 neurological beds decreased to 2812. In four counties - Bács, Heves, Tolna and Vas - only a single neurological ward survived. The capacity withdrawn from inpatient care was not transferred into outpatient services. In 2009 there were 179 hospitals and 419 independent outpatient centers in Hungary. Of the 179 hospitals 55 had neurological beds and a further 42 hospitals offered only outpatient neurological service. Neurological outpatient service is offered in Hungary altogether by 185 institutions: 97 hospitals and 88 independent outpatient centers. Suboptimal outpatient services (less than 30 hours per week) cover 57% of the outpatient capacities. There is an over fivefold difference among counties in capacities: the number of inhabitants per hospital bed ranges between 2167-13 017, and the number of inhabitants per one neurologist outpatient hour between 495-2663. In 2009 there were 1310 board certified neurologists in Hungary, of these only 834 participated at least once during the year in exclusively neurological service, and there was a large difference in workload among individual neurologists. The gross mean income of a 30-hour-per-week average neurological outpatient practice based on performance reports was 871 thousand HUF (about 4350 USD or 3160 EUR) per month. In recent years the neurological capacities significantly decreased and fragmented, do not correspond regionally to the number of population to be served, and their profitability does not cover the conditions of self sufficient operation. This analysis will help health care providers and decision makers to recognize and address the current problems and design the neurological health care system for the coming years.]
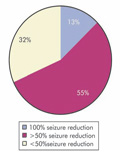
[Our clinical experience with zonisamide in resistant generalized epilepsy syndromes]
[Purpose - Zonisamide is licensed in the European Union for adjunctive therapy for partial epilepsy, but its efficacy in generalized epilepsy was less explored. Methods - This prospective observational study included 47 patients (mean age 29 years, range 3-50) with different resistant generalized epilepsy syndromes: idiopathic generalized syndromes (IGE) 15 patients, (juvenile myoclonic epilepsy four, absence epilepsy four, myoclonic absence two, unclassified IGE five), progressive myoclonic epilepsy type 1 (PME1) four, severe myoclonic epilepsy of infancy (SMEI) three, borderline SMEI three, Lennox-Gastaut syndrome/secondary generalized epileptic encephalopties 23 patients. All patients were followed up for at least six months. The mean dose given was 367 mg/day (range 100-600 mg/day), the patients received at least one and no more than two concomitant AE. Response was defined as more than 50% seizure reduction or seizure freedom. Results - The best effect was achieved in PME one, all the patients were responders. Myoclonic seizures were reduced 80%, none of the patients had generalized tonic clonic (GTC) seizures. In two of the four patients all other antiepileptics were tapered of (including piracetam), so they were GTC seizure and almost myoclonia free on zonisamide only. Responder rates were in GEFS ± SME 62.5%, in resistant IGE 62.5%, and in epileptic encephalopathies 33.3% patients. Tolerance after initial efficacy developed in six patients. Adverse effects were mild: weight loss, somnolence and confusion were repeatedly reported. Three patients reported cognitive improvement. Conclusion - Clinical benefit of a broad spectrum antiepileptic zonisamide extends across seizure types, ages and epilepsy syndromes. The efficacy in PME proved to be excellent.]
[Antinociception by endogenous ligands at peripheral level]
[It is well known that a multitude of ligands and receptors are involved in the nociceptive system, and some of them increase, while others inhibit the pain sensation both peripherally and centrally. These substances, including neurotransmitters, neuromodulators, hormones, cytokines etc., may modify the activity of nerves involved in the pain pathways. It is also well known that the organism can express very effective antinociception in different circumstances, and during such situations the levels of various endogenous ligands change. Accordingly, a very exciting field of pain research relates to the roles of endogenous ligands. The peripheral action may possibly be extremely important, because low doses of the endogenous ligands may reduce pain without disphoric side-effects, and without the abused potential typical of centrally acting ligands. This review provides a comprehensive overview of the endogenous ligands that can induce antinociception, discusses their effects on different receptors and focuses on their action at peripheral level. We found 17 different endogenous ligands which produced antinociception after their topical administration. The results suggest an important direction for the development of pain strategies that focus on the local administrations of different endogenous ligands.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
3.
4.
5.