The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2007;60(11-12)
Content
[THE ROLE OF CHRONIC BRAIN HYPOPERFUSION IN THE PATHOGENESIS OF ALZHEIMER'S DISEASE - FACTS AND HYPOTHES]
[In Alzheimer’s disease, which belongs to the neurodegenerative disorders, the ethiopathogenetic role of several risk factors has been proved. A considerable number of them are mainly known as cardiovascular risk factors and can precipitate chronic brain hypoperfusion. Using functional imaging techniques, this hypoperfusion and the resulting hypometabolism become detectable in the watershed areas of the brain as early as in the stage of mild cognitive impairment. Hypoperfusion leads to the degeneration of capillaries in this area causing the deterioration of diffusion. The further reduction of nutrient and oxygen support of neurons is capable to initiate a neurodegenerative process which spreads along the glutamaterg system arising from the neurons of the association cortices. The neuropathological lesions of this neuronal system, such as the neurofibrillary tangles and the β-amyloid plaques, are known to be the characteristic markers of Alzheimer's disease. In our review we present the development of hypoperfusion and its consequences in the watershed areas of the brain and describe the neurodegenerative process of the neuronal system arising from the neurons of the association cortices in the early stage of Alzheimer's disease. Considering the previous hypotheses and the neuropathological lesions of Alzheimer's disease we give a new consensus model to characterize the pathomechanism of the disorder.]
[GENETIC BACKGROUND OF HUMAN PRION DISEASES]
[acquired. The human prion protein gene (PRNP) is located to chromosome 20 (20p12-ter). Mutations and polymorphisms in the PRNP are associated with prion disease. Genetic prion diseases are inherited in an autosomal dominant trait, examination of the penetrance is restricted to mutation E200K (59-89%). Mutations can be substitutions or insertions. Genetic prion diseases are classified according to the clinicopathological phenotype and comprise genetic Creutzfeldt-Jakob disease, Gerstmann-Sträussler-Scheinker disease and fatal familial insomnia. Base pair insertions may resemble Creutzfeldt-Jakob disease or Gerstmann-Sträussler-Scheinker disease phenotypes, however, their unique clinicopathological presentations are also emphasized. Among the polymorphisms of the PRNP, the one at codon 129 is the most important, where methionine or valine may be encoded. This polymorphism is known to influence the phenotype of disease forms. Molecular classification of sporadic Creutzfeldt-Jakob disease also depends on the codon 129 polymorphisms in addition to the Western blot pattern of the protease resistant prion protein. According to this at least six well characterised forms of sporadic Creutzfeldt-Jakob disease are known. Influence of other genes were also investigated. Contrasting results are reported regarding the role of apolipoprotein E allele ε4, but presence of allele ε2 seems to influence the prognosis. Polymorphisms in the doppel gene or ADAM10 could not be clearly associated with Creutzfeldt-Jakob disease. Polymorphisms in the upstream and intronic regulatory region of the PRNP gene may be a risk factor for Creutzfeldt-Jakob disease. The PRNP codon 129 polymorphism was examined in non-prion diseases. Some studies suggest that this polymorphism may have influence on the cognitive decline and early onset Alzheimer’s disease.]
[HUMAN PRION DISEASES: THE HUNGARIAN EXPERIENCE]
[Background - Sporadic Creutzfeldt-Jakob disease is the most frequent human prion disease. Genetic forms are associated with mutations in the human prion protein gene (PRNP) and thought to comprise 5-15% of cases. Acquired forms include iatrogenic and variant Creutzfeldt-Jakob disease. The latter is associated with the bovine spongiform encephalopathy. We recently reported the high incidence of genetic Creutzfeldt-Jakob disease in Hungary. Materials and methods - In the present study we summarize the results of a widened investigation comprising Creutzfeldt-Jakob disease cases collected in the National Institute of Psychiatry and Neurology, Hungary in the last 12 years. We examined the disease forms and their geographical distribution. Results - Our study involved 155 patients. The four major results are as follows: 1. In Hungary we detected only sporadic and genetic forms of human prion disease, while iatrogenic and variant Creutzfeldt-Jakob disease were not observed. 2. The proportion of genetic prion disease (E200K mutation), similarly to Slovakia, is higher than reported worldwide. Our observations indicate that at least every third case is genetic Creutzfeldt-Jakob disease. The mean incidence of genetic Creutzfeldt-Jakob disease (0.42/million) is unusually high. Especially the year 2006 was striking when the incidence of genetic Creutzfeldt-Jakob disease was 1.4/million. 3. More than half of genetic Creutzfeldt-Jakob disease cases lack a positive family history. 4. Some counties and the eastern part of Hungary shows elevated incidence of human prion disease. Conclusions - Differences in the geographical distribution may be related to migration and historical relationship with the Slovakian population. Based on the increased incidence of E200K mutation, genetic testing of the PRNP is recommended in all cases with atypical neuropsychiatric disorder or suspicion of prion disease.]
[OUR EXPERIENCES WITH ANTERIOR CERVICAL CAGES AND SPACER]
[Objectives - Between 2001 and 2005 86 patients were treated for cervical disc herniations and spondylosis at our department. Stabilization was performed with different cervical cages or spacer after discectomy and decompression. The aim of the study was to examine the changes of the patients’ pain, quality of life and work ability, fusion rate, the intervertebral disc height, changes of under and upper segments and finally curvature of cervical spine. Patients and methods - Patients were followed by the authors, clinical examination, lateral and antero-posterior radiographic examinations were performed. They were asked to fill in a questionnaire, concerning their pre- and postoperative pain, quality of life and work ability. The patients’ pain was graded using a 10-point analog scale (VAS) and with a simplified, McGill-Melzak analog scale. The quality of life was measured with a 10-graduated analog scale as well. Results - More than 77% of our patients appeared at follow up examination. The fusion rate was 89.3%, operated spaces were held in 61%. In the upper segment of operated space 7%, and in the under-segment 14% were found increasingly degenerated. The curvature of cervical spine of the patients’ were 64.51% lordotic, 27.42% straight and 8.07% kyphotic. On average the patients’ pain changed on VAS from 8.179 to 5.015; on McGill-Melzak scale from 3.89 to 2.80; quality of life changed from 8.045 to 5.463. Conclusion - By the advantage of using cages, the operative approach has become smaller than before, consequently the operative pain has become less too. In addition operation time and hospital stay were significantly shorter (p<0.005) than using traditional operation approach. The majority of the patients, pain was decreased, quality of life got better. Despite this fact only 3 patients continue their original work and 5 patients do easier work. The majority of our patients were disabled before the operation, but from that time many of them became disabled, in some cases the grade of disability increased. There can be some reasons for it: the majority of the patients have other diseases for example: lumbar spondylosis and disc herniation, hypertension, diabetes, asthma and depression. There is just a few possibility of work for the disabled people. To conclude, with some of the patients, their disability means “the way out” from unemployment. These facts do not decrease the importance and usefulness of this method. Our results with this type of operation are very similar to the international statistics. This method seems to be applicable and useful.]
[UNALTERED MRNA EXPRESSION OF CALCITONIN-LIKE RECEPTOR AND RECEPTOR ACTIVITY MODIFYING PROTEINS IN HUMAN ARTERIES IN STROKE AND MYOCARDIAL INFARCTION]
[Calcitonin-like receptor (CL-R) is a functional CGRP1- receptor when complexed with RAMP1 or an adrenomedullin-receptor or when complexed with RAMP2 or RAMP3. This study was carried out 1. to set up a method to examine the relative quantity of mRNA of CL-R, RAMP1, RAMP2 and RAMP3 in human coronary (CA), pulmonary (PA) and middle cerebral arteries (MCA), and 2. to examine the level of mRNA expression in cerebro- and cardiovascular diseases. The method was validated with respect to the use of postmortem tissue and we compared β-actin and GAPDH as housekeeping genes. There was no time-dependent change in total RNA and level of mRNA for β-actin or GAPDH could be detected in vessels removed from 1 and 5 days post mortem. The expression of β-actin appears lower in coronary artery than in pulmonary artery and middle cerebral artery with no significant difference for GAPDH; both worked well. There were some differences in mRNA expression for CL-R (higher) and RAMP3 (lower) in middle cerebral artery compared to coronary artery and pulmonary artery. There was no significant difference in mRNA for RAMP1 and RAMP2 in the three types of arteries. We did not observe any difference in mRNA for CL-R and RAMPs in arteries from patients with hemorrhagic stroke, arteriosclerosis and acute myocardial infarction when compared to patients without these diagnoses. Thus the mRNA expression seems to be unaltered in these disorders.]
[BILATERAL “OVER THE TOP” DECOMPRESSION THROUGH UNILATERAL LAMINOTOMY FOR LUMBAR AND THORACIC SPINAL CANAL STENOSIS]
[Objective - The standard surgical procedures used in degenerative thoracic and lumbar spinal canal stenosis allows decompression of the neural structures by unroofing the spinal canal, often resulted in destruction or insufficiency of facet joints, sacrifice the interspinosus/supraspinosus ligament complexes and stripping of the paraspinal muscles altering an already pathologic biomechanical milieu causing segmental instability. Various less invasive techniques exists to save the integrity and prevent the instability of the spine and allow decompression of neural structures located in the spinal canal. The authors discusses the experiences with technique of unilateral laminotomy for bilateral decompression. Methods - The unilateral laminotomy for bilateral decompression technique was performed at 60 levels in 51 patients to decompress the symptomatic degenerative stenosis of the thoracic and lumbar spinal canal. The inclusion criteria were used as follows: symptoms of neurogenic claudication and/or radiculopathy, myelopathy, neuroimaging evidence of degenerative stenosis and absence of instability. Symptoms were considered refractory to nonsurgical conservative management or myelopathy was detected. Results - The distribution of mostly affected segments were the L 4-5 (45%) and L3-4 (28.4%). Neurogenic claudication and walking distance improved during the follow up period in all patients. Seven patients (13.73%) reported excellent, 32 (62.74%) good, 12 (23.53%) fair outcome and no patient a poor overall outcome. The low back pain was the major residual postoperative complaint. 25 (49%) patients were very satisfied with their outcome, 23 (45.1%) were fairly satisfied, 2 (3.9%) were not very satisfied and 1 (2%) patients was dissatisfied. Conclusion - The unilateral laminotomy for bilateral microdecompression technique minimizes resection of and injury to tissues not directly involved in the pathologic process, while affording a safe and through decompression of neural structures located in a degeneratively stenotic spinal canal.]
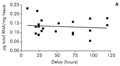
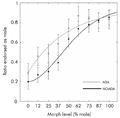
[CATHODAL TRANSCRANIAL DIRECT CURRENT STIMULATION OVER THE PARIETAL CORTEX MODIFIES FACIAL GENDER ADAPTATION]
[Previous studies have observed that prolonged adaptation to a face will bias the perception of a subsequent one. This phenomenon is known as figural or face after-effect. Although currently the topic of face adaptation enjoys utmost popularity, we still don't know much about the neural process underlying it. The aim of the present study was to determine, using transcranial direct current stimulation (tDCS), how the retinotopically organised primary visual cortex (V1) and higher-level, non-retinotopic right lateral temporo-parietal areas interact with facial adaptation processing. Seventeen healthy subjects recieved 10 min anodal, cathodal or sham stimulation over these areas during a facial adaptation task. Cathodal stimulation of the right temporo-parietal cortex reduces the magnitude of facial adaptation while stimulation over the V1 results in no significant effects. These data imply that mainly lateral temporo-parietal cortical areas play role in facial adaptation and in facial gender discrimination, supporting the idea that the observed after-effects are the result of high-level, configurational adaptation mechanisms.]
[DIFFUSION TENSOR AND FUNCTIONAL MR IMAGING OF SEVERE TRAUMATIC BRAIN INJURY AT LOW MAGNETIC FIELD]
[Aim of the study - Presentation of diffusion tensor imaging (DTI) performed at low magnetic field (1 Tesla) in the algorithm of work-up of a patient suffering from severe traumatic brain injury (TBI). Method - DTI and functional MRI (fMRI) were applied at 1 Tesla for visualization of neural pathways and examination of sensory functions of a patient with severe TBI. DTI-measurement was also performed on a healthy patient for comparison. Results - DTI acquired at low magnetic field yielded appropriate visualization of neural pathways. DTI confirmed the results of the clinical and fMRI examinations in the patient suffering from severe TBI. Conclusion - An optimized DTI can be useful in the examination of patients with TBI, moreover, it may also help in the establishment of diagnoses of other central nervous system diseases affecting neuronal pathways. The presented results suggest that DTI of appropriate quality can be performed at low magnetic field.]
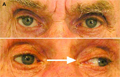
[ONE-AND-A-HALF SYNDROME - TWO CASES]
[One-and-a-half syndrome is characterized by combination of the clinical features of unilateral horizontal gaze palsy and internuclear ophthalmoplegia. The common symptoms are double vision and oscillopsia. The lesion is located in the paramedian pontine reticular formation, involving the centre of horizontal gaze and medial longitudinal fasciculus. More extensive brainstem damage may result in additional neurological signs. The most frequent underlying diseases are vascular insults, multiple sclerosis, and brainstem tumor. We present two cases of one-and-a-half syndrome. Both patients had lacunar infarction in the paramedian pontine tegmentum, revealed by MRI. The first patient had isolated eye movement disorder, while the second had additional nuclear-type facial paresis. In the first case brainstem evoked potentials indicated brainstem damage, in the second patient it was normal. Ocular symptoms improved within some days in both patients.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.