The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Hungarian Immunology - 2002;1(02)
Content
[Changes in the signal transduction of T-lymphocytes caused by hyperglycemia]
[AIMS - Lately the altered calcium balance of different cell types (eg.: erythrocytes, platelets, neutrophil granulocytes) was described in diabetes mellitus. It is also known that patients with diabetes mellitus suffer from various infections more often then healthy individuals because of immunological malfunctions. But the mechanism of these changes is still unclear. In order to investigate the effect of hyperglycemia on the function of immunocompetent cells we established an in vitro diabetes model by culturing human T cells (Jurkat cells) at different glucose concentrations for one week. Then we measured the basal cytosolic calcium level, the calcium signal after ionomycin or anti-CD3 treatment and the tyrosinephosphorylation of signal transducing proteins as well as the fructosamine level of cellular proteins. MATERIALS AND METHOD - Cytosolic free calcium levels were detected by flow cytometry using ion selective fluorescent indicator (Fluo-3 AM). Calcium signals of Jurkat cells were measured after ionomycin or monoclonal anti-CD3 antibody (OKT3) treatment. We also measured the tyrosine-phosphorylation on flow cytometer after anti-CD3 stimulation using indirect immunfluorescent labeling with monoclonal antiphospho- tyrosine antibody. The non-enzymatic glycation of cellular proteins was determined by measuring the fructosamine levels of cell lysates. RESULTS - The higher concentration of extracellular glucose resulted in concentration-dependent elevation of basal cytosolic free calcium level in Jurkat cells. Reduced calcium signal (activation capacity) was measured either after ionomycin or monoclonal anti-CD3 antibody treatments in cells kept at hyperglycemic conditions. In addition, the time kinetics of calcium signal following anti- CD3 activation was found prolonged in the hyperglycemic cells. The tyrosine-phosphorilation of hyperglycemic Jurkat cells also proved to be impaired. High glucose concentrations in tissue culture medium caused increase in the glycation of T-cell proteins. CONCLUSIONS - We propose that increased glycation of proteins involved in calcium transport and/or intracellular signal transduction of T-cells may account for our observations.]
[Anti-synthatase syndrome]
[The idiopathic inflammatory myopathies (IIM) are autoimmune diseases, characterized by symmetric proximal muscle weakness. Over the last several decades, many abnormalities of the cellular and humaral immune systems of IIM patients have been described. Some of these are autoantibodies unique to the IIM (the myositis specific autoantibodies MSA). The MSAs are antigen-driven, arise months prior to the onset of myositis, correlate in titre with disease-activity. Studies in the recent years proved that clinically and immuno-geneticaly different disease entities can be defined using myositis specific auto-antibodies. Their use make the serological classification. Myositis specific autoantibodies make it possible to define more homologies subgroups within polymyositis/dermatomyositis that may support the adequate treatment. The most common MSA is the antihistidyl- transfer RNA synthetase (anti-Jo-1), which can be found in 5-30% of patients with myositis. Patients with anti-synthatase antibodies tend to have characteristic clinical presentation of fever, small joint arthritis, intestinal lung disease, Raynaud's phenomenon, mechanic's hands and severe myositis. Sera of 65 PM/DM were tested for anti-Jo- 1 antibody. 15 patients (23%) had anti-Jo-1 antibody (10 PM, 5 DM). The patients with anti-Jo- 1 antibody has a significantly higher incidence of interstitial lung disease, arthritis, fever and Raynaud's phenomenon. These patients needed not only corticosteoid therapy, but other immunosupressive treatment. All 15 patients presented with the onset of weakness between February and July. The determination of myositis-specific autoantibodies has produced more homogenous grouping within the polymyositis/dermatomyositis patients.]
[Autoimmun thyroiditis presence in patient with Hodgkin’s disease in remission]
[INTRODUCTION - It is known that the incidence of hypothyroidism is higher in long term survivor patients with Hodgkin's disease, and it is supposed to be the result of treatment, such as neck radiotherapy. The author believe that other etiologic factors may also play a role in the development of hypothyroidism. PATIENTS AND METHODS - Looking for the possible causes of hypothyroidism, the thyroid function of 151 patients treated for Hodgkin's disease since 1970 were examined. These patients with Hodgkin's disease in complete remission for at least one year and their data on thyroid autoantibody positivity [antithyroid peroxidase antibody (aTPO), antihuman thyroglobulin antibody (aHTG), TSH antireceptor antibody (TRAK)] were analysed. RESULTS - Among the patients with antibody positive 26 received ultrasound scanning and fine needle aspiration cytology of the thyroid, which confirmed autoimmun thyroiditis. There were no significant differences between the mean age, histologic subtypes and stage of the disease between the patients with antibody positive those with antibody negative. A significantly greater number of women in the group of antibody positive patients was found and thyroid dysfunction (two cases of hyper, and 13 cases of hyperthyroidism) was revealed in 53.6% of the patients. Though antibody positivity was more frequent in patients having been treated by neck irradiation, but no significant relationship was found between the form of Hodgkin’s disease treatment and the development of thyroiditis. Thus the authors cannot confirm the assumption according to which the autoantigens released from the thyroid gland damaged by neck irradiation for Hodgkin's disease would provoke the development of thyroiditis. Since - independently of the type of treatment received - the incidence of thyroiditis is higher in patients with Hodgkin's disease, it is probable that immune regulation disorders may also play a role in its development and thus hypothyroidism is the result of a multi-factor process. DISCUSSION - These results underline the importance of a regular control of thyroid hormones and thyroid autoantibodies in follow up Hodgkin’s disease patients. Levothyroxine administered as an isohormone treatment may inhibit the development of hypothyroidism in patients with thyroiditis may improve the quality of their life.]
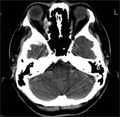
[Ocular myositis]
[INTRODUCTION - Dermato-/polymyositis is an autoimmune disorder, which belongs to the idiopathic inflammatory myopaties. It involves skeletal muscles in form of weakness and inflammatory infiltrates. Characteristic skin lesions are present in dermatomyositis. Other organs may also be affected mainly in the presence of myositis specific autoantibodies. The inflammation usually involves the proximal muscles of extremities. CASE REPORT - In the present work we report the case of a 52-year-old woman. In the previous history the removal of rectal adenocarcinoma was remarkable in 1994. After that she received chemotherapy. She complied for severe headache and pain in the right eye in 2000 October, therefore a skull CT was performed, indicating thickening of rectus medalis muscle within orbital cavity. There was an enhancement of contrast material in the muscle. Glaucoma was excluded. Neurologist suspected the presence of myositis and indicated 0.5 mg/kg corticosteroid therapy. Soon after the left eye became painful, but due to the corticosteroid treatment both eyes became painless. A control orbital CT was completely negative in 2000 November. Immunology consultancy revealed a mild proximal muscle atrophy in both lower extremities, but CPK and LDH enzyme levels were normal, EMG was characteristic for mild chronic nerve lesion. The biopsy, taken from the involved proximal muscle of lower extremity, did not show inflammatory infiltration. Complete screening for cancer was negative. Thyroid gland disease could be excluded. Immune laboratory data were negative, autoantibodies, including anti-Jo1, could not be detected. Based on the results a rare disease, ocular myositis was diagnosed. Considering the clinical improvement, the withdrawal of corticosteroid therapy was offered. Stringent immunology and oncology follow-up is required. CONCLUSION - In relation to our case report, we discuss clinical symptoms of orbital myositis, diagnostic procedures to identify the disease and also differential diagnostic considerations.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
3.
4.
5.