The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Specialities
Cardiology
[Chronic kidney disease and venous thromboembolic events]
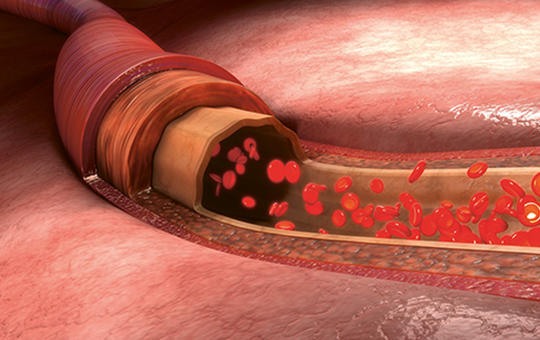
[Our aim is to analyse venous thromboembolic events regarding chronic kidney disease. Based upon epidemiologic data, both thromboembolic and haemorrhagic events are more frequent among patients with chronic kidney disease. Changes in levels of coagulant factors, thrombocyte and endothel disfunction, uremic toxins and dialysis related issues share role in pathogenesis. Guidelines lack of adequate information regarding this specific patient group. Therapeutic shift can be observed from vitamin K antagontists toward direct oral anticoagulants, not only in general population but also in CKD patients, with special interest in apixaban. Another therapeutic trend is change from unfractioned heparin to low molecular weigh heparins with anti Xa level monitoring among CKD population. Special attention is needed for thrombotic events related to eritropoietin therapy and hemodialysis access.]
[Difficulties in recognising and treatment of lower extremity arterial disease in the elderly]
[
Cardiovascular disease is the most important cause of morbidity and mortality in elderly individuals worldwide. Lower extremity arterial disease is a diffuse degenerative process by atherosclerosis of the concerning arteries that can narrow or completely block the lumen of the arteries. One of the most important risk factors is the age, thus the occurrence of lower extremity arterial disease increases significantly with it exceeding 20% over the age of 70. The incidence of lower extremity arterial disease is mounting worldwide and one of the reasons for is the increase in the average age of the population. Recognition and also treatment of the disease show elderly characteristics, the knowledge of which is important in caring for increasing population of elderly patients with lower extremity arterial disease. Early detection and corresponding preventive treatment have a significant role also in this population. The wider range of intervention options can also provide an opportunity for elderly high-risk patients to avoid amputation and get a better quality of life.]
[Lipid-lowering therapy in hypertension: what, how much and when?]
[Hypertension and dyslipidemia are two main risk factors for cardiovascular diseases. Hyperlipidemia and hypertension co-exist in a large proportion of patients. Furthermore, people dealing with hyperlipidemia and hypertension are at a higher risk of developing cardiovascular diseases than those who suffer from hyperlipidemia or hypertension. Therefore, an essential aspect of hypertension therapy is the management of hyperlipidemia as it can prevent the progression of atherosclerosis and related macrovascular events such as myocardial infarction and stroke. Previous studies have demonstrated that 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor statins were associated with an unexpected reduction in blood pressure in hypertensive patients. Fibrates and omega-3 fatty acids may also improve the efficacy of antihypertensive treatment. These pharmacological approaches have a favorable effect on both lipids and blood pressure thresholds. These treatments hold great promise in preventing cardiovascular complications in this unique population.]
[Statin therapy in kidney patients: what, how much and when?]
[The association between an elevated cholesterol value and the risk of cardiovascular disease is well known. Over decades various classes of drugs were introduced to decrease cholesterol levels, but the real breakthrough came with the use of statins. In the population without renal disease numerous studies have proven statins to be effective in decreasing the level of lipids, in reducing cardiovascular risk, in delaying atherosclerosis and in the regression of plaque. Similarly, in the population with renal disease, many studies have justified the role of statins in reducing CV risk, especially in mild-moderate renal failure, but also in the population of patients requiring dialysis. Studies have also proven their effectiveness in slowing the progression of renal failure and in the reduction of proteinuria. They might also play a protecting role in contrast material-, aminogylcoside-, cardiac- surgery-induced acute kidney injury. Both the cardiac and the renoprotective effectiveness can be explained by summary of their lipid-decreasing and pleiotrop effects. Based on the increased CV risk proven in the population with renal disease, chronic kidney disease is in the high and very-high risk group in national and international guidelines. Reaching the determined lower target values in the high risk and very high risk group is only possible via aggressive antilipemic treatment. Out of statins, molecules capable of intensive decreasing of lipid levels are in favor, in case of ineffectiveness or even from start ezetimib (an agent inhibiting cholesterine uptake) can be added.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.