The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Hungarian Radiology - 2010;84(04)
Content
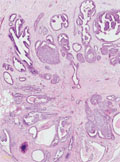
[Lesions resembling radial scar of the breast - Is preoperative biopsy of the radial scar needed?]
[INTRODUCTION - The radial sclerosing lesion is one of the most common benign breast lesions. It can mimic malignant tumours on mammogram in many cases. In one third of the cases invasive tumour or in situ carcinoma occur in radial sclerosing lesion, therefore surgical excision is mandatory. The aim of our work is to diagnose the malignant cases with preoperative biopsy (FNAB, core biopsy) when radial scar morphology lesion is detected in order to avoid two-step surgical procedure. PATIENTS AND METHODS - Forty-five patients were examined with the same method. In all cases of radial sclerosing morphology lesions a mammography, complementary radiograms, ultrasonography (US) and synchronous US guided FNAB and core biopsy were performed. Postoperative pathological findings were compared to the results of preoperative biopsies. RESULTS - In 6 of 45 cases (13%) malignant tumours mimicked radial scar in morphology. All of them were diagnosed preoperatively with core biopsy (B5). The FNAB was nondiagnostic (C1) in 2 patients, suspicious for malignancy (C4) in 2 patients and was positive in 2 cases (C5). Radial scars or complex sclerosing lesions were diagnosed in 39 patients preoperatively. In 28 cases (72%), malignancy was not detected with postoperative pathological examination. In 8 cases (20%) DCIS and, in 3 cases (8%), malignant tumours were found associated to radial scar. Neither FNAB nor core biopsy gave false positive results in the non-malignant group. In the patients with DCIS associated to radial scar, core biopsy proved malignancy in 5 cases and FNAB in only 1 case. In 3 cases of invasive malignant tumour associated with radial scar core biopsy was positive in 1 patient, while FNAB was negative or non-diagnostic in all of them. CONCLUSION - According to the latest publications vacuum- assisted large-core needle biopsy (VLNB) performed with 11G needle (12) is the safest procedure to justify or exclude malignancy in the radial scar. Observation would be enough in the non-malignant cases and this procedure has therapeutic potential as well. In case where these methods are not available, as in Hungary, all radial scar cases require surgical excision. Therefore, preoperative core biopsy is recommended in order to avoid a two-step surgical procedure.]
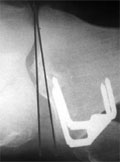
[The effect of the orientation of the distal femur on the correction of axis after closing-wedge high tibial osteotomy - Short-medium term radiological assessment]
[Introduction - High tibial osteotomy (HTO) is a generally accepted treatment for medial unicompartmental osteoarthritis of the knee with varus alignment. The clinical result is affected by the correction of the varus malalignment. The degree of correction appears to be dependent not only on correction performed on tibia but also on the orientation of the distal femur. The valgus orientation of the distal femur can be associated with postoperative over-correction and varus orientation of the distal femur with postoperative under-correction. Patients and methods - We performed radiological assessment of 82 knees preoperatively and after closing wedge high tibial osteotomy (CWO) in the 10th postoperative week, in the 12th postoperative month and at the time of the final follow-up (23-54 months) on a standing weight-bearing anteroposterior radiograph. Pre- and postoperatively we measured the orientation of the distal femur, described as the lateral angle between the anatomic axis of the femur and the distal articular surface of the femur (FC-FS). We subdivided the knees into 3 groups based on the orientation of the distal femur. In group A the FC-FS was 83-85° (normal orientation of the distal femur), in group B the FC-FS was £82° (valgus orientation of the distal femur) in group C the FC-FS was ³86° (varus orientation of the distal femur). Pre- and postoperatively we measured the lateral angle between the anatomic axis of the tibia and the proximal articular surface of the tibia (TP-TS) and the lateral angle between the distal articular surface of the femur and the proximal articular surface of the tibia (the articular component of the varus deformity FC-TP) in all groups. We determined the anatomical femorotibial angle (FTA) as a sum of FC-FS, TP-TS and FC-TP. Results - In the first ten postoperative weeks - with significant osseous correction happened in the three groups - the articular component also decreased significantly in groups A and B, but did not change in group C. Between the postoperative 10th and the final follow-up examinations we did not notice significant osseous correction loss in any groups. In groups A and B the articular correction loss was not significant, at the same time in group C we noted significant articular correction loss. Conclusion - At valgus orientation of the distal femur the CWO results in greater correction of the limb’s anatomical axis than the osseal correction performed on the tibia. This additional correction equals the (preoperatively unpredictable) amount of the articular correction. At varus orientation of the distal femur the CWO results in less correction of the limb’s anatomical axis than the osseal correction performed on the tibia. This difference equals the (preoperatively unpredictable) loss of articular correc- tion.]
[Necrotizing enterocolitis in neonatology: comparing the role of X-ray and ultrasonographic examinations]
[INTRODUCTION - The authors’ purpose was to analyse the role of abdominal ultrasonography (US) in the diagnosis of necrotizing enterocolitis (NEC). They have compared the sensitivity of the current standard diagnostic modalities for this clinical entity: plain abdominal radiography and abdominal US. For a more objective comparison, they created an US scale along with utilising the score system based on abdominal radiography which was published recently. PATIENTS AND METHODS - 46 out of 76 neonates having both clinical and radiological diagnosis of NEC had comparable radiographic and sonographic examinations between June 2006 and October 2009. The authors created a 10-grade US score system, in which sonographic signs of NEC are listed in order of severity, corresponding, where possible with the radiographic scale that was available. The findings were scored individually, then the distribution of scores and their relationship to each other were analysed. For further analysis four groups of severity based on the scores were created with the following categories: mild, moderate, severe and very severe. After graphical representation of the groups, the relationship of the groups created on the basis of scoring the findings by the two diagnostic methods were examined. RESULTS - According to this analysis both abdominal radiographs and sonographs are suitable for diagnosing NEC, which has been justified with statistical data. When analysing the severity groups the authors proved that the two methods diverge in judging groups 3 and 4, thus severe and very severe. The distributions of severity groups formed by the two imaging modalities are different, (P<0,01); and the proportion of group 3 and group 4 is different in case of US and radiographic examinations (P=0.003). CONCLUSIONS - Abdominal sonography and radiography are equally suitable diagnostic methods for diagnosing NEC, and the two methods match each other very well. In cases of mild state, the severity of the disease was found to be the same with both methods, but US allows more sensitive differentiation of serious cases. It is very sensitive in detecting perforations, so it could play a role in determining the indication of surgery.]
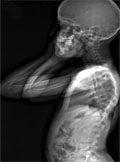
[Surgical treatment of scoliosis: pre- and postoperative follow-up with whole-body EOS radiography]
[Currently, Cotrel-Dubousset spondylodesis is the treatment of choice in orthopaedics. It allows for correction of deformity in three-dimensions allowing for stable fixation. EOS (Extended Orthopedic System) is an ultra low dose X-ray imaging system, simultaneously acquiring images of the whole body in two planes. Examinations with the EOS system is not only indicated in cases related to orthopaedics but in multiple other conditions owing to its low level of emitted radiation with rapid and cost-effective imaging. The importance of EOS examination is emphasized in systemic skeletal disorders, thus allowing itt o be used in various other clinical fields.]
[Investigation of colon-transit in children with chronic idiopathic constipation]
[Constipation is a very common problem in childhood with diverse etiology. Most of the cases can be attributed to functional constipation. The types of chronic idiopathic constipation (CIC) are as follows: slow colonic transit, functional fecal retention, combination of the two and constipation which is predominant in irritable bowel syndrome. The first step in diagnosing/treating the condition should involve the exclusion of primary organic causes, as well as metabolic, neurological and iatrogenic ones. Then special anorectal physiological investigations are needed. In our laboratory, the aim of radionuclide study is to demonstrate the two types of CIC, the slow colon transit (SCT) and the functional fecal retention (FFR). Such evaluation makes it easier for the clinician to plan appropriate treatment. The radionuclide study is conducted as follows: after adequate pretreatment, Tc-99m Fyton is administered orally, and images are collected at 2, 6, 12, 24, 30 and 48 hours following administration. After the evaluation of the specific studies, exploration of the causes and exact diagnosis are established. Appropriate treatment is always planned individually. We would like to demonstrate this by presenting 3 cases.]
[Inflammatory myofibroblastic tumor in rare abdominal localisation]
[INTRODUCTION - Inflammatory myofibroblastic tumor is a rare entity. The etiology and pathomechanism of this tumor is still unknown. In most of the cases it behaves as a benign or locally recurrent tumor and does not metastasize, but because of its aggressive local growth it can be judged malignant. For an accurate diagnosis adequate imaging (CT, MR), invasive intervention which is usually surgical excision and pathologic or histological examination must be performed. CASE REPORT - A case of a 19 year old woman is presented who was diagnosed by a CT scan with a 4 cm tumor in the midline of the upper third of the abdominal cavity. After surgical excision the inflammatory myofibroblastic tumor was confirmed after the pathological inspection. CONCLUSION - Despite that inflammatory myofibroblastic tumor is infrequent in virtue of the clinical picture and imaging exams we have to take this disease into account. The misdiagnosis can lead to unnecessary invasive interventions and psychological effort for the patient which could be avoided by the cooperation of the different subspecialties and thoroughgoing medical examination.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
3.
4.
5.