The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Hungarian Radiology - 2009;83(01)
Content
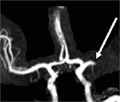
[Self-expanding metallic stents in intrahepatic biliary strictures after liver transplantation]
[INTRODUCTION - Bile duct complications remain a key problem of liver transplantation. Two main types are recognized: anastomotic and intrahepatic. In cases of anastomotic strictures good results can be achieved with surgery or minimally invasive therapy. Intrahepatic stenosis usually requires retransplantation. In this report the results of intrahepatic metallic stent placements are analyzed. PATIENTS AND METHODS - Since 1995, 20 patients with intrahepatic bile strictures were referred for percutaneous treatment. Of 34 percutaneous transhepatic cholangiography, 33 successful drainages were performed and 58 balloon dilatations were employed to overcome. In 13 patients, 20 metallic stents were implanted. One bleeding complication was successfully treated with selective embolization. RESULTS - The average follow up time was 35 months. 14 patients have no symptoms, 12 of them after metallic stent placements and 4 of them after retransplantation (2 patients had metallic stents at retransplantation). One patient has metallic stent and an external drain waiting for retransplantation. Three patients died after 7 retransplantations. Two patients died on the waiting list, one with and one without external drain. There were no deaths after successful metallic stent placement. CONCLUSION - After meticulous preparations metallic stent placement is safe and effective in intrahepatic biliary stenosis after liver transplantation. The patients can be stabilized till the retransplantation, or it can even be avoided.]
[Xanthogranulomatous cholecystitis]
[INTRODUCTION - The xanthogranulomatous cholecystitis is a rare and benign form of lesions associated with diffuse thickening of the gall bladder wall. It is important to recognize it radiologically because it can be mistaken easily for gall bladder carcinoma. The characteristic US, CT and MR findings, however, may be helpful in the differential diagnosis. CASE REPORT - We present the cases of two middleaged female patients suffering from right upper quadrant, radiating abdominal pain for several weeks without occurrence of fever. In both patients, the ultrasound examination revealed marked thickening of the gall bladder wall containing hypoechoic nodules. Further, non-specific sign such as cholecystolithiasis and fine infiltration of the adipose tissue surrounding the gall bladder and dilatation of extrahepatic or intrahepatic bile ducts were visible. On the post contrast CT images, rim enhancement was detectable. MR/MRCP examination showed a sharp delineation of the gall bladder from the liver parenchyma. Both patients underwent cholecystectomy. The pathological examination excluded malignancy and confirmed the diagnosis of xanthogranulomatous cholecystitis. CONCLUSION - The characteristic features of xanthogranulomatous cholecystitis (hypoechoic xanthogranulomas in the markedly thickened gall bladder wall and the presence of calculi) can be detected by ultrasound examination. CT or MRI may play an important role in confirmation of the diagnosis of an inflammatory process and provide useful information in exclusion of gall bladder carcinoma.]
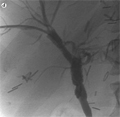
[Transjugular intrahepatic portosystemic shunt implantation in a patient with severe dilatative cardiomyopathy]
[INTRODUCTION - Indications for TIPS (transjugular intrahepatic portosystemic shunt) are usually portal hypertension induced by alcoholic or viral cirrhosis. Reported patient underwent TIPS because of a rare indication where his rapidly progressing heart failure lead to rapid deterioration of the splanchnic hypertension. CASE REPORT - A 51 years old male was admitted with severe dilatative cardiomyopathy and atrial fibrillation, generalized edema refractory to conservative treatment, and rapidly worsening hepatic laboratory test results. TIPS implantation achieved improvement of all clinical signs, decreased edema and the patient could finally be discharged. CONCLUSION - TIPS can result in improved quality of life not only in primary hepatic cirrhosis but in other clinical circumstances with portal hypertension.]
[Difficulties in the diagnosis of ectopic ureter]
[INTRODUCTION - Ureter ectopy refers to the distal opening of the ureter at the site of the bladder neck or lower. 70-80% of the ectopic ureters are associated with pyelectasia and duplicated ureters. The incidence of this is 2-3 times higher in females. CASE REPORT - Following is a case report of a boy who was diagnosed with left-sided pyelectasia during a prenatal ultrasound scan. The postnatal ultrasound revealed a duplicated pelviceal cavity and ureter. The upper pole ureter and the pelvis demonstrated dilatation. At 8 months of age a left side heminehprectomy was performed. Two years postoperatively a follow-up ultrasound revealed a dilatation of the ureteral stump on the left side, which progressed. On MCUG the ureteral stump was identified inserting on to the proximal urethra. Cystography and MR urography demonstrated a ureteral stump which inserted on to the urethra. A repeat surgery was performed to remove the stump. Patient is symptom-free ever since. CONCLUSION - In ectopic, non-refluxing ureters long-term follow-up is necessary following heminephrectomy. A ureter stump besides the bladder can cause serious diagnostical difficulties. Also, it is possible that a dilating stump may lead to a reflux not identified earlier. MCUG and MR urography can help to clear delineate the pathology.]
[A rare pancreatic mass in childhood]
[INTRODUCTION - Malignant pediatric pancreas tumors are rare in the pediatric age group. Among these tumors the malignant hemangiopericytoma is an even more rare condition. CASE REPORT - We have diagnosed this soft tissue sarcoma in a three month old infant during a screening abdominal ultrasound examination. The examination showed a space-occupying lesion in the region of the pancreas and the adrenals. Following further diagnostic imaging, a complete surgical resection was performed. Histology showed malignant hemangiopericytoma. The child received a 5 month long, successful adjuvant chemotheraphy. CONCLUSIONS - Malignant hemangiopericytoma belongs to the non-rhabdomyosarcoma group of diseases. Two subtypes have been described: infantile-type ( hemangiopericytoma) in infants under 1 year, and the adult-type disease in children over 1 year of age. About one third of the infantile subtype are considered congenital. Most common anatomic locations are the retroperitoneum, the pelvis, the extremities, the head and neck region. Prognosis is favorable, the 10-year-survival rate is 80%. Differential diagnosis includes other tumors of the region, such as lesions of the adrenal gland, kidney, stomach and pancreas.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.