The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Hungarian Radiology - 2007;81(07-08)
Content
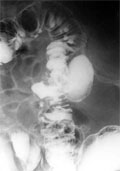
[Giant colonic diverticulum]
[INTRODUCTION - Very rarely do colonic diverticula grow enourmously - from 3-4 cm upto 15-20 cm in diameter - causing diagnostic difficulties. PATIENT AND METHODS - The authors present a case of an elderly male patient where the ultrasound examination accidentally revealed irregularity in a part of the sigmoid colon with thickened wall. This finding was then examined by colonoscopy, colonography (double contrast barium enema) and CT. Two giant diverticula, measuring 4-5 cm in diameter, arising from the sigmoid colon were demonstrated. Considering the old age of the patient and the lack of clinical symptoms, the affected part of the sigmoid colon had not been surgically resected. CONCLUSION - Giving a general overview on the pathogenesis, presentation and differential diagnosis of colonic diverticula, the authors emphasise the importance of colonography. Also, as far as the authors know, this is the first Hungarian report on giant colonic diverticulum.]
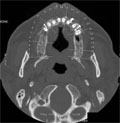
[Dental-CT imaging]
[Nowadays the widespread application of dental and oral surgical procedures and the use of dental implants established the need of special examination of the jaw. These implants are mainly made of metal and surgically imbedded into the edentulous jaw. Metallic artefacts deteriorate the diagnostic value of conventional X-ray. In the past years, the use of multislice CT technique and dental reformatting program can demonstrate structures which were hardly or not visible due to their shape and location. The aim of this review is to introduce this special dental CT program.]
[Sarcoidosis involving liver and spleen, and with hypercalcemia]
[INTRODUCTION - Sarcoidosis is a relatively common multisystemic disorder. Chest involvement is most frequent, but any organ can be involved. In case of abdominal lesions the suspicion of sarcoidosis rarely arises. CASE REPORT - A 53-year old female patient with a history of crural pain unresponsive to medications and weight loss of unknown origin was sent to the internist. Hypercalcemia and bone pain suggested multiple myeloma, however, this diagnosis could not be confirmed. Chest X-ray examination was negative. Splenomegaly and multiple hypodens splenic and hepatic lesions were detected by ultrasound and abdominal computed tomography. Finally, ultrasound guided biopsy of the liver proved stage II sarcoidosis. Steroid therapy was initiated and the splenic and hepatic lesions seen with ultrasound and CT scan disappeared. CONCLUSION - Sarcoidosis is usually suspected following chest X-ray or during chest CT examination. Nevertheless, our case demonstrates that multiple lesions in the spleen or liver may indicate sarcoidosis even in the absence of thoracic lesions. Biopsy taken from the lesions can lead to adequate diagnosis.]
[Abdominal and thoracal manifestations of posttransplantation lymphoproliferative disorder in children]
[INTRODUCTION - Posttransplantation lymphoproliferative disorder is a secondary disease of transplanted patients, usually with good response to reduction of immunsuppressive therapy. PATIENTS AND METHODS - The lymphoproliferative disorder was diagnosed in four children among 139, renal, liver and lung transplanted patients. Clinical data (original disease, transplanted organ, age and time elapsed since transplantation at the diagnosis of the disorder) and imaging findings (chest X-ray, thoracal and abdominal computed tomography scans) were analysed retrospectively. RESULTS - Thoracal and abdominal forms were the most frequent manifestations of posttransplantation lymphoproliferative disorder in our patients. Following features have been diagnosed on imaging studies: multiple liver nodules (two cases), multiple nodules in the renal parenchyma (two cases), splenomegaly (two cases), bowel wall thickening (two cases). Retroperitoneal and mesenteric lymph node enlargement was found in all patients. Thoracal manifestations were as follows: mediastinal lymphadenopathy (two cases), hilar mass (one case), multiple pulmonary nodules (one case). Renal rupture with perirenal hematoma in one case, hilar mass envolving the main bronchus in one case, hepatic abscesses necessitating drainage in one case, and bowel wall necrosis in one case were the complications of posttransplantation lymphoproliferative disorder. CONCLUSION - Presenting symptoms are aspecific, often mimicking infection. Posttransplantation lymphoproliferative disorder has to be excluded if aspecific symptoms in a transplanted patient are present, or the patient does not react properly on antibiotics. First step investigations include chest X-ray and abdominal sonography. Neck, chest and abdominal CT are mandatory for detecting all manifestations, for staging the disease and to determine the best localization of obligatory biopsy.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.