The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Oncology - 2020;7(4)
Content
[Contemporary treatment of the malignant tumors of the uterus]
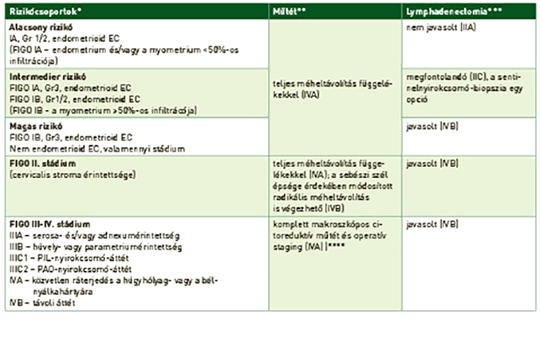
[Yearly around half a million women are diagnosed with uterine cancer worldwide, having leaded to 90,000 deaths in 2018. Endometrial cancers (ECs) are the most common forms of gynaecological malignancies, while sarcomas represent not more than 3% of uterine cancers. In 80-85% of cases ECs are low-grade and diagnosed at an early stage, therefore potentially curable by surgical procedure and postoperative radiotherapy (if necessary). However, the optimal adjuvant management of high risk ECs is still an issue and the recognition of molecular subtypes is generating further clinical investigations in the field. Surgery is also the only curative method in sarcoma-care, but evidences for adjuvant management is scarce and indefinite. Beyond therapeutic benefits, quality of life is also an important factor in modern oncology. Therefore in gynaecological oncology there are intentions like preserving fertility and ovarian function, avoiding systemic lymphadenectomy or using minimal invasive technique to improve the patients’ quality of life without the deterioration of the therapeutic outcome. In the management of advanced endometrial cancer, the biological agents have opened a new era in recent years: pembrolizumab as second line option for MSI-H/dMMR/TMB high EC and the combination of lenvatinib-pembrolizumab for MSS/pMMR EC have been approved. But there are also promising results or ongoing studies with other agents: anti-HER2 therapy for serous EC, cabozantinib-nivolumab or ipilimumab-nivolumab for carcinosarcoma, PARP inhibitors with endocrine therapy for ER positive ECs. Here I present a short summary on the current therapeutic options and the most important ongoing clinical trials in uterine cancer.]
[The highlights of the 2020 ESMO virtual congress]
[The year of 2020 brought unexpected challenges to the healthcare systems all around the globe. Every country had to reorganise their medical priorities to face the COVID19 pandemic. The practice of virtual medicine has expanded in the past years, these new circumstances have increased its speed drastically. Within these unusual circumstances we could take part in the virtual congress of the ESMO 2020 where we were able to hear about the new results of oncology to provide up-to-date care for our patients. Compared to the past years, we did not learn too many breakthrough results, the most of the novelties helped us place our experiences to their ideal place in patient care. The investigations which examined the SARS-CoV2 virus effects on oncologic patients showed grave results, the infection increases the vulnerability and mortality of patients receiving active anticancer therapies or suffering from an active cancer.]
[Tumor-agnostic therapy in oncology]
[Tumor-agnostic therapy is considered as a promising therapeutic approach in oncology, however classification, validation of the targets and standardized methodology for their evaluation is mandatory. The development and approval of the tumor-agnostic drugs should be based on biomarker driven clinical trials. To date three validated biomarkers are known, the high microsatellite instability (MSI-H), the fusion of the neurotrophic-receptor-tyrosine-kinase (NTKR) genes, and the high mutation burden (TMB-H) of the tumors. Pembrolizumab (anti-PD-1 antibody) was the first approved tumor-agnostic drug, the MSI-H status of the tumor was the first indication, then later the TMB-H status was also approved. Larotrectinib and entrectinib are approved for the treatment of NTKR fusion-positive tumours.]
[The forefront of ovarian cancer therapy: update on PARP inhibitors]
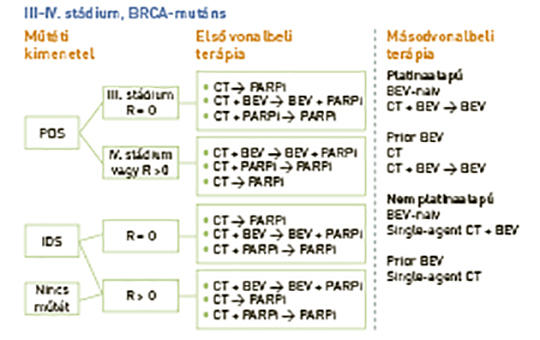
[In recurrent ovarian cancer, poly(ADP-ribose) polymerase (PARP)-inhibiting agents have transformed the treatment of platinum-sensitive disease. New data support use of PARP inhibitors earlier in the treatment algorithm. We review results from recent phase III trials evaluating PARP inhibitors as treatment and/or maintenance therapy for patients with newly diagnosed ovarian cancer. We discuss the efficacy and safety of these agents in the all-comer and biomarker-selected populations studied in clinical trials, and compare the strengths and limitations of the various trial designs. We also consider priorities for future research, with a particular focus on patient selection and future regimens for populations with high unmet need. Four phase III trials (SOLO-1, PAOLA-1/ENGOT-OV25, PRIMA/ENGOT-OV26 and VELIA/GOG-3005) demonstrated remarkable improvements in progression-free survival with PARP inhibitor therapy (olaparib, niraparib or veliparib) for newly diagnosed ovarian cancer. Differences in trial design (treatment and/or maintenance setting; single agent or combination; bevacizumab or no bevacizumab), patient selection (surgical outcome, biomarker eligibility, prognosis) and primary analysis population (intention-to-treat, BRCA mutated or homologous recombination deficiency positive) affect the conclusions that can be drawn from these trials. Overall survival data are pending and there is limited experience regarding long-term safety. PARP inhibitors play a pivotal role in the management of newly diagnosed ovarian cancer, which will affect subsequent treatment choices. Refinement of testing for patient selection and identification of regimens to treat populations that appear to benefit less from PARP inhibitors are a priority.]
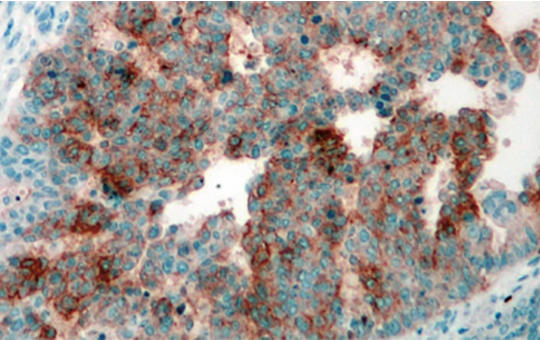
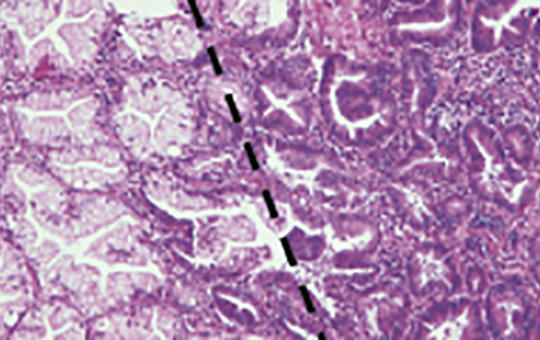
[Heterogeneity in cancer]
[The basic function of cells is to maintain a balance between proliferation and programmed cell death, which allows the cell to perform its specific function. This activity fits closely, partly with neighboring cells and partly with the intercellular population. Errors can occur in the regulation of all this, of course mutations are the most common. Some of these can cause disturbances in cell life, but most mutations do not play an important role. It is well known to distinguish between benignity and malignancy, of which metastasis of tumor cells is the real danger (in fact, a tumor can be considered malignant clinically if it forms metastasis in hematological tumors rather than solids) and this polyclonality interferes with cellular function. It is understandable, therefore, that these two phenomena, metastasis and selection, can be considered the primary targets of therapy. Heterogeneity plays an important role in cell life.]
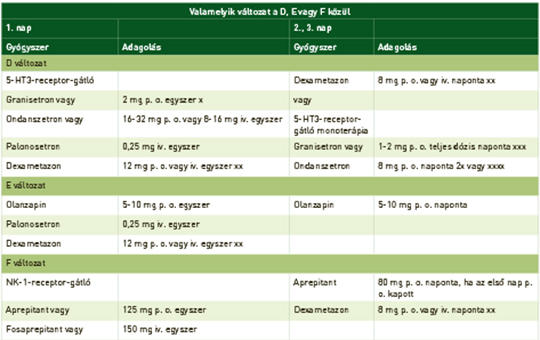
[The antiemetic treatment of oncologic procedures]
[Nausea and vomiting are multistep pathway controlled by the brain. The emetic impulses come form cortex, as a psyhotic reaction or throught nervus vagus. In the medulla in the area postrema are the specific nuclei concerning to the emetic episodes. Most important neurotransmitters are the serotonin, substance P and dopamins. The chemotherapeutic drugs caused the emesis and vomiting at different frequences. The effect of 5-HT3 and NK-1 receptor antagonist have not are the most important antiemetic role. The fixed oral combination: netupitant and palonosetron (NEPA) increase instead of ensure the patient adherence. Guidelines recommend the antiemetic combinations in different types of chemotherapy. This rewiev covers the specific nausea and vomitig forms: breakthrough, multiday chemotherapy induced, radiation induced and anticipatory emesis. We summarise also the antiemetic therapy in childhood.]
[Side effects of CT scans]
[Computed tomography (CT) scans which result in relatively high doses of radiation exposure, but have an indisputable diagnostic advantage, are becoming more common among radiological diagnostic imaging procedures. Based on the linear no-threshold model of stochastic radiation effects, even the lowest radiation dose suffered can trigger the formation of tumors. Tumor formation due to radiation exposure during CT scans, thanks to their higher radiation sensitivity and longer life expectancy, mainly affect youngsters. Most epidemiological studies on the subject concluded that CT scans increased the risk of leukemia and brain tumor development in young people in a dose-dependent manner. However, absolute tumor numbers are not really significant, so if appropriately indicated, examinations should be performed as soon as possible. CT scans of the lower abdomen in pregnant women may lead to developmental abnormalities in the fetus. In the vast majority of cases, only a series of CT scans can result in larger than 100 mGy fetal exposures which may raise the potential of abortion. The physician performing the examination is responsible for the justification and optimization of imaging studies involving radiation exposure.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.