The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2015;68(07-08)
Content
[The role of β-amyloid and mitochondrial dysfunction in the pathogenesis of Alzheimer’s disease]
[Alzheimer’s disease is the most common form of dementia in mid- and late life. The 7-10% of the population over 65 and the 50-60% of the population over 85 are affected by this disease. On the contrary of its prevalence the pathogenesis of the disease is not well defined and there is no effective neuroprotective therapeutic agent. Three predominant neuropathological features of the Alzheimer’s disease brain are intracellular neurofibrillary tangles consisting mainly of the hyperphosphorylated protein t; the extracellular amyloid deposits (neuritic plaques) consisting of amyloid b peptide; and the extensive neuronal cell loss in the hippocampus and in portions of the cerebral cortex. The possible reason of the extensive neuronal cell loss can be the mitochondrial dysfunction observed in Alzheimer’s disease. Beyond the unclarified pathogenesis the causality of these characteristic neuropathologic phenomena are still unknown. In this study we would like to deal with two actual hypotheses, with the amyloid cascade and with the mitochondrial cascade hypotheses. We try to give an overview of these two hypotheses and to depict their interrelationship.]
[Radiosurgery of intracerebral cavernomas - Current international trends]
[Although still a controversial management option, radiosurgery of intracranial cavernomas has become increasingly popular world-wide during the last decade. Microsurgery is a safe and effective treatment for symptomatic hemispheric cavernomas. However, the indication for microsurgical resection of deep eloquent cavernomas is relatively limited even in experienced hands. The importance of radiosurgery has recently been appreciated in parallel with increasing positive experiences both in terms of effectiveness and safety, especially for cases high risk for surgical resection, in the brainstem, thalamus and basal ganglia. While radiosurgery was earlier indicated mainly for surgically inaccessible lesions that had bled multiple times, a more proactive policy has recently become more accepted. In our opinion preventive treatment with the low morbidity radiosurgery serves the patients’ interest especially for deep eloquent lesions that had bled not more than once, due to the cumulative morbidity of repeated hemorrhages. Despite our increasing knowledge on natural history, there is currently no available treatment algorithm for cavernomas. Arguments for all three treatment modalities (observation, microsurgery and radiosurgery) are established, but their indication criteria are yet to be defined. It is time to organize a prospective population based data collection in Hungary, which appears to be the most realistic way to clarify indication criteria.]
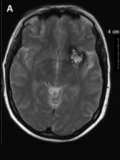
[Radiosurgery of intracerebral cavernomas - Current Hungarian practice]
[Background and purpose - Radiosurgery is an increasingly popular treatment option especially for deep eloquent intracerebral cavernomas that are often too risky for surgical removal, but their re-bleed carries significant risk for persisting neurological deficit. Gamma-radiation based radiosurgery has been being available since 2007 in Hungary in Debrecen. Our aim is to summarize our experience accumulated during the first five years of treatment and to compare it to the international experience. Patient selection and methods - We retrospectively analyzed 51 cavernomas in 45 patients treated between 2008 and 2012 in terms of localization, natural history, and the effect of radiosurgery on re-bleed risk and epilepsy, and its side effects. Results - We treated 26.5% deep eloquent (brainstem, thalamic/basal ganglia) and 72.5% superficial hemispheric cavernomas. The median presentation age was 25 years (13-60) for deep, and 45 years (6-67) for superficial cavernomas. They were treated median of 1 year after presentation. 64.5% of deep cavernomas bled before treatment, the annual risk of first hemorrhage was 2%/lesion, re-bleed risk 21.7%, with 44% persisting morbidity. 13.5% of superficial cavernomas bled prior to treatment, the risk of first bleed was 0.3%, there was no re-bleed, and 35% caused epilepsy. We used GammaART-6000TM rotating gamma system for treatment, marginal dose was 14 Gy (10-16), and treatment volume 1.38-1.53 cm3. Re-bleed risk of deep eloquent lesions fell to 4% during the first two years after treatment and to 0% thereafter, and no hemorrhage occurred from superficial lesions after treatment. Persisting morbidity in deep lesions came from adverse radiation effect in 7% and from re-bleed in 7%, and there was no persisting side effect in superficial cavernomas. 87.5% of cases of epilepsy resistant to medical therapy improved. Radiological regression was found in 37.5% and progression in 2% after treatment. Conclusions - Radiosurgery of cavernomas is safe and effective. Early preventive treatment for deep cavernomas carrying high surgical risk is justified. Moreover, for superficial lesions that are surgically easily accessible radiosurgery also appears to be an attractive alternative.]
[Neurointerventional treatment of acute ischemic stroke: the Kaposvár experience]
[Aim of the study - In the present study, we report procedural and mid-term functional outcome data on the first 50 neurointerventional treatments of acute ischemic stroke in the Kaposi Mór County Hospital, Kaposvár, Hungary. Materials and methods - Endovascular recanalization of occluded large cervical and intracranial arteries was performed following an unsuccessful intravenous lysis or when intravenous lysis was contraindicated. A control cohort was retrospectively formed by analyzing data of 16 patients who has been unsuccesfully treated with iv. lysis before neurointervention was available in our hospital. Results and conclusion - Recanalization rate was 84% and major complication rate was 2% in the neurointerventional group. Mid-term good functional outcome, defined as mRS 0-2, was achieved in 44% in the neurointerventional and in 13% in the intravenous lysis group, after 11.5 and 39.7 months follow-up period, respectively. Subgroup analysis revealed patient age as the strongest predictive factor of good functional outcome. Our data shows that neurointerventional treatment of acute ischemic stroke gives substantially improved functional outcome, in accordance with the results of the recently published international randomized trials.]
Mental health of physicians - nationwide representative study from Hungary
Background and aim - Somatic and mental health and stress factors of physicians became an issue of growing interest in both national and international researches. Our aim is to give an overviewing analysis of Hungarian physicians’ mental health state. Methods - Representative, cross-sectional, quantitative survey on a representative sample of Hungarian physicians (n=4784). The control group was formed by the population group of a national survey conducted by “Hungarostudy 2013” (n=2000). Results - Suicidal thoughts (18.8% vs. 9.6%, p<0.001), the scores of Somatic Symptom Scale (PHQ-10, 20.4% vs. 13.6%, p<0.001) were significantly higher among physicians. The suicidal attempts (1.9% vs. 3.5%, p=0.053) and BDI depression scores (7.9% vs. 29.5%, p<0.001) were significantly higher in the control group. High Perceived Stress Scale (PPS) scores occurred in 43.3% of the physicians sample, and 43.4% of them had high scores in the Athenian Insomnia Scale (AIS). The young (<35) female physicians showed significantly higher rates of suicidal thoughts, higher scores of PHQ and PPS. In the young female cohort, the AIS scores were significantly higher than of the other physicians. Conclusions - Mental health of physicians (sleep disorders, suicidal thoughts and psychosomatic symptoms) showed poorer results than the population data. BDI scores and the rate of suicidal attempts showed favourable trends. The next step in the physicians’ mental health researches is to investigate the most decisive risk factors, and to work out the prevention tools.
Thrombocytopenia with gabapentin usage
Gabapentin is an antiepileptic drug approved for adjunctive therapy for partial seizures. We report a case of a patient who had thrombocytopenia with the dose of 2400 mg/day of gabapentin. The causal relationship between gabapentin and thrombocytopenia was revealed by dramatic increase in thrombocyte count following the cessation of the gabapentin treatment. To our knowledge, this is the first case report with a hematopoietic side effect of gabapentin.
[Treatment of post spondylodesis adjacent segment disease with minimally invasive, anterolateral surgery on lumbar spine: there is no need for dorsal operation?]
[Adjacent segment disease (ASD) occurs with a probability of 30% in the lumbar spine following spinal fusion surgery. Usually advanced degenerative changes happen cranially to the fused lumbar segment. Thus, secondary spinal instability, stenosis, spodylolisthesis, foraminal stenosis can lead to the recurrence of the pain not always amenable to conservative measures. A typical surgical solution to treat ASD consists of posterior revision surgery including decompression, change or extension of the instrumentation and fusion to the rostral level. It results in a larger operation with considerable risk of complications. We present a typical case of ASD treated surgically with a new minimally invasive way not yet performed in Hungary. We use anterolateral abdominal muscle splitting approach to reach the lumbar spine through the retroperitoneum. A discectomy is performed by retracting the psoas muscle dorsally. The intervertebral bony fusion is achieved by implanting a cage with large volume that is stuffed with autologous bone or tricalcium phosphate. A cage with large volume results in excellent annulus fibrosus tension, immediate stability and provides large surface for bony fusion. A stand-alone cage construct can be supplemented with lateral screw/rod/plate fixation. The advantage of the new technique for the treatment of ASD includes minimal blood loss, short operation time, significantly less postoperative pain and much less complication rate.]
[LGI1 encephalitis: the first Hungarian patient]
[In the recent years, it has been increasingly recognised that in a group of limbic encephalitis antibodies are directed against the scaffolding protein LGI1 (Leucine-rich glioma inactivated 1), which is part of the voltage gated potassium channel (VGKC) complex on neural synapses. Patients present with seizures and subacute history of neuropsychiatric symptoms, including psychosis and changes in memory, cognition, behaviour. Faciobrachial dystonic seizures can be observed, which are highly characteristic for LGI1 encephalitis. MRI shows medial temporal abnormalities in more than half of the cases. CSF evaluation is usually normal. Hyponatremia is frequently associated and may confuse the initial diagnosis. Early recognition and prompt initiation of immunotherapies are of great importance. The clinical improvements often correlate with the antibody levels. We present the case of a 64-year old man, who responded quickly to plasma exchange and major improvement was noted within few weeks.]
[Focal motor seizures and status epilepticus provoked by mirtazapine]
[The seizure-provoking effect of the tetracyclic antidepressant mirtazapine is not a well-known adverse effect of the drug. The authors report on a 39-year-old non-epileptic patient who had been treated for depression with the usual daily dose of mirtazapine. Having increased the daily dose of the drug from 30 to 45 milligrams he experienced a few clonic seizures of the right lower limb. This symptom and insomnia erroneously intended the patient to further increase the daily dose of mirtazapine, which immediately resulted in the evolution of focal clonic status epilepticus in the same limb. After admission, this condition was recorded by video-EEG and abolished by intravenous administration of levetiracetam after the intravenous clonazepam had been ineffective. Discontinuation of mirtazapine and administration of carbamazepine resulted in completely seizure-free state that persisted even after carbamazepine treatment was terminated. The clinical and laboratory data indicate the seizure-provoking effect of mirtazapine in the reported case.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.