The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2015;68(05-06)
Content
[Zonisamide: one of the first-line antiepileptic drugs in focal epilepsy ]
[Chronic administration of antiepileptic drugs without history of unprovoked epileptic seizures are not recommended for epilepsy prophylaxis. Conversely, if the patient suffered the first unprovoked seizure, then the presence of epileptiform discharges on the EEG, focal neurological signs, and the presence of epileptogenic lesion on the MRI are risk factors for a second seizure (such as for the development of epilepsy). Without these risk factors, the chance of a second seizure is about 25-30%, while the presence of these risk factors (for example signs of previous stroke, neurotrauma, or encephalitis on the MRI) can predict >70% seizure recurrence. Thus the International League Against Epilepsy (ILAE) re-defined the term ’epilepsy’ which can be diagnosed even after the first seizure, if the risk of seizure recurrence is high. According to this definition, we can start antiepileptic drug therapy after a single unprovoked seizure. There are four antiepileptic drugs which has the highest evidence (level „A”) as first-line initial monotherapy for treating newly diagnosed epilepsy. These are: carbamazepine, phenytoin, levetiracetam, and zonisamide (ZNS). The present review focuses on the ZNS. Beacuse ZNS can be administrated once a day, it is an optimal drug for maintaining patient’s compliance and for those patients who have a high risk for developing a non-compliance (for example teenagers and young adults). Due to the low interaction potential, ZNS treatment is safe and effective in treating epilepsy of elderly people. ZNS is an ideal drug in epilepsy accompanied by obesity, because ZNS has a weight loss effect, especially in obese patients.]
[Alemtuzumab: benefits and challenges of new therapy in multiple sclerosis]
[The widening spectrum of MS treatment is partially due to increasing knowledge about the pathogenesis of MS. The humanized monoclonal antibody against CD52, alemtuzumab has been approved in Europe for the treatment of MS, which results in long-term depletion of B and T cells due to complement- and antibody-mediated cytotoxicity. Based on phase 2 and 3 clinical trials, alemtuzumab decreases the risk of sustained neurological deficit and progression compared to high-dose subcutaneous interferon- β1a in patients with active relapsing-remitting MS, either treatment-naïve or with breakthrough disease. We review advantages and benefits of the treatment, discuss safety concerns, and present a case to describe practical issues.]
[Characteristics and differential diagnostics of sleep related pathological movements. Update 2013]
[Wide variety of the movements (from the physiologic body position changes to different pathologic events) can be seen during the sleep period. The most important types of these movements are the sleep related events (from the parasomnias to the restless leg related movements), the movement disorders and the epilepsy related events. To differentiate between these events is required special skill, which is based on appropriate characterisation of the events (for example timing, repetition, pattern), the polysomnographic and video-EEG examination and validated questionnaires (FLEP scale). The appropriate differential diagnostics and therapy must be based on the knowledge of the relationship of the sleep architecture and movement events. This review would like to provide guideline for the understanding and recognizing the nature of the sleep related movements.]
Chronic cerebrospinal venous insufficiency - disease or misdiagnosis?
Background and purpose - Former studies reported internal jugular vein stenosis in patients with multiple sclerosis. We aimed to evaluate if these venous stenoses were real and cerebral venous outflow of patients with multiple sclerosis differed from that of normal controls. Methods - 20 controls were prospectively investigated by angiography and duplex ultrasound. Seven patients with multiple sclerosis underwent angiography in other centers; we reviewed these registrations and performed venous ultrasound examinations. Results - Angiography displayed >50% stenosis of internal jugular vein in 19 controls (69±17% on the right and 73±13% on the left side) and <50% stenosis in 1 control (43.5% and 44.6%). All 7 patients had at least one-sided stenosis. The mean degree of stenosis was 63±16% on the right and 67±13% on the left side. There was no significant difference in the degree of stenosis between patients and controls. However, these “stenoses” disappeared if the contrast agent was injected at a catheter position below the orifice of the subclavian vein during venography. The venous flow volume was also similar between groups: 479.7±214.1 and 509.8±212.0 ml/min (right and left side) in the patients and 461.3±224.3 and 513.6±352.2 ml/min in the control group; p=0.85 and 0.98 (right and left). Color and power duplex imaging also revealed normal blood flow of the internal jugular vein in all patients and controls. Conclusion - The cerebral venous status of patients with multiple sclerosis and controls were similar. The angiographic “stenoses” were virtual, caused by the contrast dilution effect of the non-contrast blood stream of the subclavian vein.
[Validation of the Hungarian Unified Dyskinesia Rating Scale]
[Background - The Unified Dyskinesia Rating Scale (UDysRS) was published in 2008. It was designed to be simultaneous valid, reliable and sensitive to therapeutic changes. The Movement Disorder Society organizing team developed guidelines for the development of official non- English translations consisting of four steps: translation/back-translation, cognitive pretesting, large field testing, and clinimetric analysis. The aim of this paper was to introduce the new UDysRS and its validation process into Hungarian. Methods - After the translation of UDysRS into Hungarian and back-translated into English, it was reviewed by the UDysRS translation administration team. Subsequent cognitive pretesting was conducted with ten patients. For the large field testing phase, the Hungarian official working draft version of UDysRS was tested with 256 patients with Parkinson’s disease having dyskinesia. Confirmatory factor analyses (CFA) determined whether the factor structure for the valid Spanish UDysRS could be confirmed in data collected using the Hungarian Official Draft Version. To become an official translation, the Comparative Fit Index (CFI) had to be ≥0.90 compared to the Spanish-language version. Results - For the Hungarian UDysRS the CFI was 0.98. Conclusion - The overall factor structure of the Hungarian version was consistent with that of the Spanish version based on the high CFIs for the UDysRS in the CFA; therefore, this version was designated as the Official Hungarian Version Of The UDysRS.]
[Acoustic CR®-neuromodulation - first experiencies in Hungary with novel patented method in therapy of chronic subjectiv tinnitus]
[Objective - Acoustic CR®-neuromodulation is a novel patented method for the therapy of chronic subjective tinnitus and has been tested in Hungary, as one of the first European countries introducing this procedure. It can be used for the treatment of monaural or binaural tonal tinnitus. Suitability of patients for this therapy was assessed by the help of an appropriate set of criteria. Aim of our study was to analyze 6-month therapy and related measurement data of patients first treated with this method in Hungary and evaluate the results. Method - 27 outpatients (20 males, seven females) with a minimum of 6-month long history of subjective tinnitus were assessed (four detected on the right side, six on the left side, 17 on both sides) who were treated for six months by Acoustic CR®-neuromodulation. On 44 treated ears (21 right, 23 left), changes of tinnitus frequency and loudness were measured and analysed, using Visual Analogue Scale (VAS) loudness/annoyance/pitch scores and Tinnitus Handicap Inventory tests, which were performed at defined intervals during the treatment period. Results - During this 6-month treatment period, significant decrease was detected in tinnitus frequency and loudness by tinnitometry (irrespective of the affected side), and an improvement in VAS annoyance/pitch scores and THI test results. VAS loudness did not show any significant changes. Conclusion - Acoustic CR®-neuromodulation therapy may be a useful treatment of subjective chronic tinnitus, but its efficacy should be proved in controlled clinical trials.]
Altered BOLD response within the core face-processing network in congenital prosopagnosia
Background and purpose - Congenital prosopagnosia is a life-long disorder of face perception. To study the neural backgrounds of congenital prosopagnosia we measured the blood oxygen level-dependent response of congenital prosopagnosic participants, using functional magnetic resonance imaging. Methods - We tested three persons of the family (father, daughter and son), having symptoms of congenital prosopagnosia, as well as healthy controls, using combined neuropsychological and functional magnetic resonance imaging methods. To reveal the neural correlates of the impairments, blood oxygen level-dependent responses within the occipito-temporal cortex were measured to faces and nonsense object images in a block-design experiment. Results - Neuropsychological tests demonstrated significant impairments of face perception/recognition in each subject. We found that the activity of the fusiform and occipital face areas as well as of the lateral occipital cortex was significantly reduced in congenital prosopagnosic participants when compared to controls. Analysis of the hemodynamic response function revealed a lower peak response, but also a significantly faster and stronger decay of the blood oxygen level-dependent response in the occipito-temporal areas in congenital prosopagnosic participants when compared to controls. Conclusion - Our results emphasize the dysfunction of the core face processing system, as well as the lateral occipital complex, in congenital prosopagnosia. Further, the functional impairment of these areas is signalled best by the altered hemodynamic response function, showing abnormally low initial peak and stronger and faster decay in the later parts of the blood oxygen level-dependent response.
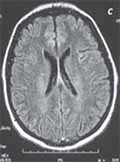
Watershed infarction in hypereosinophilic syndrome: a diagnostic dilemma in FIP1L1-PDGFR alpha-associated myeloid neoplasm
Introduction - The FIP1L1-PDGFR alpha-positive, hypereosinophilic syndrome (HES) is a new category of hematological entities. Various clinical symptoms may occur, with no specific characteristics in either the clinical picture or the neuroimaging findings, and this may give rise to a diagnostic dilemma. A report on a long follow-up period (10 years) in a case of HES that presented with neuropsychiatric symptoms appears to be unique. Besides the complexity of the diagnostic process, the successful treatment is discussed. Case report - The HES was diagnosed in a male patient at the age of 33 years, with involvement of the central nervous system and the myocardium. After the onset of the clinical signs, the MRI indicated bilateral cerebral and cerebellar cortico-subcortical lesions involving the watershed areas, mainly in the parieto-occipital regions. High-dose intravenous steroid (methylprednisolone 500 mg/day) alleviated the neurological symptoms within a few weeks, and the administration of imatinib (200 mg/day) resulted in an impressive regression of the hypereosinophilia and splenomegaly within 6 weeks. During the follow-up, the patient has continued to receive imatinib. The molecular remission has persisted, no new complaints have developed and the condition of the patient has remained stable. Conclusion - The timely recognition of the HES and identification of the disease subtype which led to the administration of imatinib may be the key to successful treatment. The long stable follow-up period gives rise to a new dilemma in the treatment of the HES in these special cases: for how long should a patient receive a tyrosine kinase inhibitor, and may the treatment be suspended?
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
3.
4.
5.