The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2013;66(11-12)
Content
[Treatment possibilities in advanced Parkinson’s disease]
[In the course of Parkinson’s disease, advanced and late stages can be distinguished. In the advanced stage, levodopa has good effect on motor symptoms, but patient care is often hindered by levodopa-induced complications such as motor fluctuation and dyskinesias. In the late stage levodopa response becomes poor, falls, dementia and psychotic symptoms appear and patients often need hospitalization. In the advanced stage, the quality of life may be improved better by device-aided therapy than by best oral medical treatment. The alternatives are apomorhin pump, levodopa carbidopa intestinal gel with pump and deep brain stimulation. The therapy plan should be based on the principle: “the right treatment, to the right patient, in the right time”.]
[Status epilepticus and its treatment - Update 2013]
[Our study provides an overview of the results and guidelines published on the treatment of status epilepticus in the last five years. In recent years, as a result of scientific observations and collected data, the definition of and treatment approach to status epilepticus have been refined and novel therapeutic methods have been developed. The updated guidelines provide guidance in everyday medical practice. However, only a relatively small number of randomized studies are available on status epilepticus, especially in second-line treatment and third-line treatment, thus it is difficult to transfer the newest methods into clinical practice and into updates to treatment protocols. Due to the nature and epidemiology of the disease, the treatment of status epilepticus remains a daily challenge for healthcare providers. The key points of an effective treatment are: expeditiously initiating appropriate therapy, concurrent causal treatment and anticonvulsant therapy, early detection of nonconvulsive status epilepticus, as well as avoiding "overtreatment" and side effects.]
[Psychosis as a process - New implications of staging models of schizophrenia]
[The article discusses contributing factors in the pathogenesis of schizophrenia. In the last fifteen years, the emphasis has shifted from curative to prodromal and premorbid characteristics of later schizophrenia patients. Nevertheless, most studies are limited to the area of early detection and intervention of schizophrenia with much fewer focusing on actual prevention. A more general preventive approach not limited to psychotic condition is clearly underestimated. Following a review of current literature on prodromal approaches and identified premorbid markers of schizophrenia, the article outlines a possible trajectory of later psychotic condition with detectable, distinct stages from birth on. Based on this extended staging model involving neurotoxic impact and early prefrontal-limbic dysfunction, it argues for a refined, phase-specific treatment protocol including preventive interventions. Accepting a model of schizophrenia as an illness with detectable, phase-specific signs and symptoms from infancy on leads to the need to implement preventive interventions. Through this approach, we could, in the optimal case, be able to identify early signs of neuromotoric and cognitive dysfunction not specific for psychosis. Furthermore, it would be useful to lay greater emphasis on the detection of these early signs in the training of health care professionals. This approach calls for a close cooperation between psychologists, psychiatrists, neuropsychologists and special education experts and a change in the way we view psychotic illness.]
[Post-operative management of primary glioblastoma multiforme in patients over 60 years of age]
[Background and purpose - Optimal treatment for elderly patients with glioblastoma multiforme is not well defined. We evaluated the efficacy of post-operative radiotherapy with or without concomitant and/or adjuvant temozolomide in patients aged ≥60 years to assess survival and identify prognostic factors of survival. Methods - A retrospective analysis of overall survival and progression-free survival in patients with newly diagnosed glioblastoma multiforme aged ≥60 years treated with postoperative radiotherapy with or without temozolomide chemotherapy was conducted at our institutions. Prognostic factors were determined by univariate and multivariate analyses. Results - Of 75 study participants (54.7% male; median age at first diagnosis, 65.1 years), 29 (38.7%) underwent gross total resection, whereas others underwent partial resection or biopsy only. All but 1 patient received radiotherapy. Twenty patients received concomitant temozolomide only. Adjuvant temozolomide (1-50 cycles) was administered in 42 patients; 16 received ≥6 cycles. Median overall survival was 10.3 months. One- and 2-year overall survival rates were 42.6% and 6.7%, respectively. Median progression-free survival was 4.1 months. Radiochemotherapy was generally well tolerated. Median overall survival was 15.3 and 29.6 months for patients who received 6-12 cycles and >12 cycles of adjuvant temozolomide, respectively. There were no significant differences in overall survival between age groups (60-64, 65-69, and ≥70 years). Adjuvant temozolomide, Karnofsky performance status ≥70, and additional surgery after progression were significant prognostic factors of longer overall survival (p<0.05). Conclusions: Radiochemotherapy, including ≥6 cycles of adjuvant temozolomide, was safe and prolonged survival of glioblastoma patients aged ≥60 years. Aggressive therapy should not be withheld from patients aged ≥60 years with good performance status because of age.]
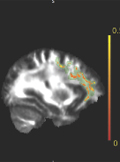
[Diffusion MRI measured white matter microstructure as a biomarker of neurodegeneration in preclinical Huntington’s disease]
[Background - Huntington’s disease is a progressive neurodegenerative disease, genetically determined by CAG trinucleotide expansions in the IT15 gene. The onset of the symptoms is related to the number of CAG triplets. Because the patients are asymptomatic in the early phase of the disease, in vivo biomarkers are needed to follow up the neurodegeneration and to test putative neuroprotective approaches. One such promising biomarker is the diffusion MRI measured microstructural alteration of the white matter. Methods - Seven presymtomatic, mutation carriers and ten age-matched healthy controls were included in the study. Diffusion parameters were compared between groups and correlated with measures describing neurodegeneration. In order to reduce the possible misregistration bias due to atrophy the analysis was restricted to the core of each fibre bundles as defined by maximal fractional anisotropy (Tract- Based Spatial Statistics). Results - Decreased fractional anisotropy, along with increased mean, parallel and perpendicular diffusivity was found in white matter tracts, mainly in the corpus callosum. An inverse correlation was detected between the fractional anisotropy and neurodegeneration score (derived from the number of CAG triplets and the patient age) from the areas of the left precentral gyrus, frontal lobe, corpus callosum and the capsula extrema. Altered diffusion parameters are promising biomarkers of the neurodegeneration in Huntington’s disease.]
[Assessment of the role of multidrug resistance-associated proteins in MPTP neurotoxicity in mice]
[Goals - The available scientific data indicate that the pathomechanism of Parkinson's disease (PD) involves the accumulation of endogenous and exogenous toxic substances. The disruption of the proper functioning of certain transporters in the blood-brain barrier and in the blood-cerebrospinal fluid barrier in PD would accompany to that accumulation. Although there is an emerging role of the dysfunction of multidrug resistance-associated proteins (MRPs), members of ATP-binding cassette (ABC) transporter superfamily, in neurodegenerative disorders, there is only a few available data as regards PD. So the aim of our study was the assessment of the role of certain MRPs (1,2,4 and 5) in neurotoxicity induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP). Methods - Following the intraperitoneal administration of silymarin (with MRP1, 2, 4 and 5 inhibitory effects), naringenin (with MRP1, 2 and 4 stimulatory effects), sulfinpyrazone (with MRP1, 4 and 5 inhibitory and MRP2 stimulatory effects) and allopurinol (with MRP4 stimulatory effect) in doses of 100 mg/kg, 100 mg/kg, 100 mg/kg and 60 mg/kg, respectively, for one week before and after the administration of MPTP in C57B/6 mice in acute dosing regimen, the striatal concentrations of dopamine, 3,4-dihydroxyphenylacetic acid and homovanillic acid has been measured using high-performance liquid chromatography. Results - Although the results of these experiments showed that neither of these substances exerted significant influence on MPTP-induced striatal depletion of dopamine and its metabolites, naringenin exerted a slight prevention of dopamine decrease, while allopurinol considerably enhanced the MPTP-induced lethality in mice. The explanation of these findings would be that the stimulation of MRP1- and MRP2-mediated transport of glutathione conjugates of toxic substances may have slight beneficial effects, while stimulation of MRP4-mediated efflux of brain urate, which has an important antioxidant potency, may worsen the effects of oxidative stress.]
[The fate of tyrosinaemic Hungarian patients before the NTBC aera]
[Before the introduction of the NTBC treatment (Orfadine) from two tyrosinemic Hungarian families 1-3 tyrosinemic homozygous male patients died of hepatocellular carcinoma and one patient of hepatocellular carcinoma combined with clear cell renal adenocarcinoma. From the third tyrosinemic family one homozygous girl patient has been treated with NTBC (Orfadine), IMTV-AM, she is symptom-free. Her molecular genetic mutations analysis in the FAH gene detected a common intronel mutation, affecting splicing and of predicted severe effect, IVS6-1 g > t/IVS6-1 g > t with systemic name c.456-1 g > t/c.456-1 g > t (Prof. Magdalena Ugarte).]
[Big blind spot syndrome (papillophlebitis) with unusual visual field defect]
[We present three cases, where young patients had unilateral disc edema with normal optic nerve function. We diagnosed their disease as big blind spot syndrome (BBSS). What is remarkable, however, is that in two of the three cases the extent of the visual field defect considerably exceeded the one regularly emerging in BBSS, which caused us some difficulty in differential diagnosis. The characteristics and the differential diagnostic questions of the big blind spot syndrome are summarised and we would like to draw attention to this unusual, but probably not very rare, form of it.]
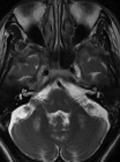
[Reversible hepatocerebral degeneration-like syndrome due to portovenous shunts]
[Ataxia and tremor are rare manifestations of hepatocerebral degeneration due to portovenous shunts. Ammonia is a neurotoxin that plays a significant role in the pathogenesis of hepatic encephalopathy. A 58-year old male patient was assessed with the complaints of gait disturbance, hand tremor, and impairment of speech. His neurological examination revealed dysarthric speech and ataxic gait. Bilateral kinetic tremor was noted, and deep tendon reflexes of the patient were hyperactive. Serum ammonia level was found to be 156.9 μg/dL. Cranial magnetic resonance (MR) imaging revealed increased signal intensity in bilateral globus pallidus on T1-weighted axial sections, and bilateral prominent hyperintense lesions in the middle cerebellar peduncles on T2-weighted axial sections. On his abdominal MR portography, multiple portohepatic venous collaterals were noted in the right and left lobes of liver parenchyma in 2D FIESTA axial MR sections. To our knowledge, we reported the first case of acquired hepatocerebral degeneration presenting with cerebral symptoms without any hepatic findings in which clinical improvement was noted, and hyperammonemia disappeared following medical treatment.]
[Comparative efficacy of different muscle relaxants in the rehabilitation of post-stroke patients with spasticity]
[Comparative efficacy of different muscle relaxants in the rehabilitation of post-stroke patients with spasticity 2013;66(11-12)]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.