The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Clinical Neuroscience - 2005;58(07-08)
Content
[Frontotemporal dementia - Part II Differential diagnosis, genetics, molecular pathomechanism and pathology]
[This is a comprehensive paper in three parts covering history, prevalence, clinical forms, differential diagnosis, genetics, molecular pathomechanism, pathology, clinical diagnosis and treatment of frontotemporal dementia (FTD). The second part focuses on the differential diagnosis, genetics, molecular pathomechanism and pathology. The clinical diagnosis of frontotemporal dementia is based on the presence of a prominent disturbance of the executive function and of frontal lobe syndrome or a progressive aphasic syndrome without severe global cognitive impairment. Of other dementias, it is primarily Alzheimer’s disease that it should be differentiated from, but other psychiatric disorders must also be ruled out. The disease has familial and sporadic forms. Recent identification of mutations in the gene encoding the microtubule-associated tau protein in the inherited frontotemporal dementia and parkinsonism linked to chromosome 17 (FTDP-17) has demonstrated that various tau dysfunctions can lead to neurodegeneration. Tau gene mutations have varied effects on the biology and function of the protein. This heterogeneous pathomechanism explains the wide range of clinical and neuropathological features observed in the FTDP-17. Tau and ubiquitin antibodies can be detected by sensitive immunohistochemical methods. The diagnosis of FTD should be based on neuropathological examination, and this is also the only method by which it can be definitely differentiated from other types of dementias.]
[ELECTROPHYSIOLOGICAL SIGNS OF STRUCTURAL CHANGES IN MOTOR UNITS AFTER ISCHAEMIC STROKE]
[Introduction - While it is several decades ago that electrophysiological studies in the early stages after an ischaemic stroke revealed spontaneous activity in the affected muscles, today few data are available on the peripheral changes in later stages after a cerebrovascular event. The aim of this study was to detect electrophysiological signs that could indicate changes at the motor unit level occurring within a longer post-stroke period. Patients and methods - Forty-four patients who had developed hemiparesis after an ischaemic stroke in the area of the middle cerebral artery were involved in the study. Motor and sensory nerve conduction studies and electromyography were carried out on each side on six nerves and in five muscles respectively. Values between the affected and unaffected side were compared by statistical methods. Results - In patients with hemiparesis present for less then nine months, low M wave amplitudes, fibrillation potentials and an increased number of complex motor unit potentials were found on the affected side; in patients with symptoms present for more then nine months the mean duration and size index of the motor unit potentials in the paretic abductor digiti minimi muscle were increased. These data suggest a process of neurogenic type. The signs of distal axonal damage observed in the early period after stroke have been replaced later by chronic neurogenic changes. These changes could be the consequence of spinal motor neuron damage and axonal transport disturbance due to the loss of supraspinal trophic inputs. Conclusion - The correlation between the extent of electrophysiological changes and of the central motor deficit of the patient indicates the importance of delaying this process by appropriate rehabilitation procedures.]
[Increasing cerebral perfusion pressure in serious cranial injury - contradictory effects of dopamine]
[Background - Management of cerebral perfusion pressure is an important element of the treatment of traumatic brain injury. Vasopressors are accepted as a method of choice to increase mean arterial blood pressure and thus cerebral perfusion pressure in the face of rising intracranial pressure. There are, however, some unresolved issues and potential risks to this therapy. Matherial and methods - This study therefore examines the effects of dopamine on physiological changes as well as on brain edema and water content that can be readily assessed by MRI/MRS in 1. a rodent model of rapidly rising intracranial pressure, caused by diffuse injury with secondary insult and 2. a model of cortical contusion. Results - Dopamine was capable of restoring cerebral perfusion pressure in the model of rapidly rising intracranial pressure. However, this was associated with only a partial restoration of cerebral blood flow. In the brain tissue two profiles of change in the apparent diffusion coefficient of water (ADCw) were seen; one in which ADCw recovered to baseline, and one in which ADCw remained persistently low. Despite that dopamine did not alter these profiles, MRI-assessed tissue water content was increased four hours after injury and dopamine increased cerebral water content in both subgroups of injury, especially in the subgroup with a persistently low ADCw (p<0,01). In the contusion group dopamine significantly worsened the edema both in the injured and in the contralateral area of hippocampus and temporal cortex even though the ADCw values did not change, except for the contralateral hippocampus, where both water content and ADCw values rose with treatment, suggesting extracellular accumulation of water. Conclusion - The results suggest that dopamine has a double effect - while it temporarily and partially restores cerebral blood perfusion, at the same time it induces an increase in brain swelling and thus an increase in intracranial pressure in some cases. It is possible that in a subgroup of patients vasopressor treatment leads to an opposite effect several hours later. Vasopressor therapy in the clinical setting therefore should be cautiously applied.]
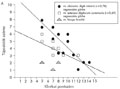
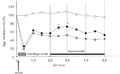
[Investigation of cerebral autoregulation in Parkinson’s disease]
[Background and purpose - The frequent orthostatic intolerance in Parkinson’s disease could be the consequence of cardiovascular autonomic failure and/or a damaged cerebral autoregulation (AR). To clarify this question the regulation of cerebral circulation was investigated by polygraphic method. Methods - On a tilt table simultaneous and continuous registrations were made of MCA velocity (VMCA) by transcranial Doppler, arterial blood pressure by non-invasive method, and end-tidal CO2, in supine and in tilted positions of 10°, 30°, 70° grades. The cerebral autoregulation was characterized by the slope of the curve of the arterial blood pressure at the level of the Willis-circle (BPW, as MCA perfusion pressure) plotted against the MCA velocity, achieved by linear regression (y=ax+b function, a=AR, or index of autoregulation). Patients - The data of 17 parkinsonian patients (PP) and eight age-matched controls (C) were analyzed. Results - The decrease of blood pressure in parkinsonian patients was significantly lower than in the controls when supine position was restored from 70° (ΔABP 70°-0°PP= -3.1±7.5 Hgmm; ΔABP 70°-0C°=-11.1±7.3 Hgmm; p<0.05), which suggests a damage to the sympathetic cardiovascular system. A disturbance of the cerebral autoregulation in patients was suggested by a progressively decreasing MCA average velocity (VMCA) during graded tilt, which was significiant at 70° (ΔVACM=9.8±8.82% cms-1; pCPP <0,05), and by a higher slope of pressure-velocity curve (ARC=0.143±0.125% cms-1/Hgmm; ARPP=0.38±0.25% cms-1/Hgmm; pC-PP<0.05). Conclusions - The results show that the cerebral blood flow of patients is more dependent on perfusion pressure compared to healthy controls. The disturbance of the sympathetic cardiovascular system and of cerebral autoregulation could be the consequence of a damage to the postganglionic structures in Parkinson’s disease. These results could explain the frequent orthostatic intolerance of patients even with normal blood pressure.]
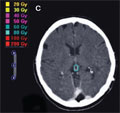
[125I brachytherapy of pineal parenchymal tumours]
[Introduction - Pineal parenchymal tumours make up 0,3% of all brain tumours. Stereotactic biopsy has by now become an indispensable method to detect these tumours and it can be safely performed. Patients and method - Two patients with pineoblastoma were treated with 125I brachytherapy. The MRI and CT images taken 15 and 18 months after irradiation showed significant tumour shrinkage. Results - Tumour volume was 0.76 cm3 in the control CT image in Case 1, a shrinkage by 73% compared to 2.87 cm3 measured at the time of planning the interstitial irradiation. In Case 2, tumour volume measured on the control MRI examination was 0.29 cm3 as opposed to 1.27 cm3 of original tumour volume, which represents a 77% shrinkage. Conclusion - The insertion of isotope seeds was performed at the same time as the biopsy, because thus the knowledge of the histological diagnosis could spare the patients from a second stereotactic intervention. The CT- and image fusion guided 125I stereotactical brachytherapy is a procedure that can be dosimetrically precisely planned and surgically accurately and safely performed.]
[Stiff-person syndrome - two Hungarian cases and review of the literature]
[The stiff-man syndrome is a rare neurological disorder characterized by progressive stiffness of the axial muscles and co-contraction of agonist and antagonist muscles sometimes accompanied by involuntary sudden muscle spasms. The disease is thought to be caused by immunological changes leading to a GABA transmission disturbance, but the precise pathogenesis is not clear. Two Hungarian cases are presented in this article accompanied by a review of the literature. The aim of the paper is to call the attention on this presumably underdiagnosed disease. The diagnostic laboratory tests of the disease are available in Hungary.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
Clinical Oncology
[Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up]3.
Clinical Oncology
[Pharmacovigilance landscape – Lessons from the past and opportunities for future]4.
5.