The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Ca&Bone - 2007;10(01)
Content
[The increase of fracture risk in type 1 and type 2 diabetes mellitus]
[Studies in the last couple of years found more and more convincing evidence about the fact that impaired glucose metabolism leads to structural changes in the skeletal system leading toward osteoporosis. While patients with type 1 diabetes mellitus have decreased bone density, measurement showed increased bone mineral density in patients with type 2 diabetes mellitus. Despite these differences, risk of vertebral and nonvertebral fractures is increased in both groups of diabetic patients. Decreased pancreatic beta cell function is accompanied by several hormonal disturbances leading to decreased bone formation even in the early stage of diabetes. Peak bone mass of diabetic children is lower than found in nondiabetic children. Late complications of diabetes, vascular and neuronal impairments, impaired renal function, and secondary hormonal disturbances are added to this process. IGF-1 may have a crucial role in the pathogenesis of osteoporosis in diabetes. The structure of the molecule is similar to insulin. IGF-1 has effect on normal bone formation, inhibits the apoptosis and interferes with several other metabolic pathways. IGF-1 mediates the effect of growth hormone to the muscular and skeletal system. IGF-1 level decreases with age, and lower level of IGF-1 is found in diabetic patients. Long term complications of diabetes can also occur, which may enhance the process of bone resorption. Although the evidence is growing that fracture risk is higher in diabetic patiens, there are still scientists who question the association between the two disorders.]
[Disturbances of the bone metabolism in type 1 diabetic patients]
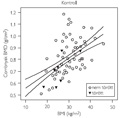
[AIMS - Because of contradictory data in literature our aim was to study bone metabolic disturbances and their correlates with anthropometric and metabolic parameters in type 1 diabetic patients (T1DM). Since quantitative bone ultrasound (QUS) measures bone qualities different from BMD, and it has only been scarcely investigated in T1DM, our aim was to describe covariates of QUS parameters. PATIENTS AND METHODS - Osteodensitometry was performed (lumbal spine, femur neck - DEXA; calcaneal ultrasound) on 115 T1DM patients (34 male, 81 female; mean age: 41.4±11 [± SD] yrs; BMI: 23.9±3.0 kg/m2; diabetes duration: 21.6±11.7 yrs; HbA1c: 8.1±1.3%). In addition anthropometric, blood pressure and laboratory parameters (HbA1c, lipids, renal function, fibrinogen, homocystein, PTH, TSH, β-CrossLaps, vitamine D3, osteocalcin, osteoprotegerin) were measured, data using a questionnaire were collected. RESULTS - The prevalence of osteoporosis was 9/112 (8%). A further 21/62 patients with osteopenia were found. Disturbances of bone metabolism have been more frequently proven on lumbal spine (p<0.001). Using multiple linear regression modelling, the independent covariates of osteopathy were systolic blood pressure, body weight, β-CrossLaps and cystatin C. The average broadband ultrasound attenuation (BUA) was 114.2±14.9 in males vs. 108.4±16.3 dB/MHz in females (p=0.07), the mean speed of sound (SOS) 1552±26 in males vs. 1559±32 m/s in females (p=0.32). SOS values in addition to bone density were associated with fracture risk. The independent covariates of BUA were body weight and height (R=0.473, p<0.001), and of SOS only fibrinogen (R=0.305, p=0.032). CONCLUSIONS - According to our results the prevalence of osteoporosis in acceptable controlled T1DM patients is relatively low. The more common metabolic calcipenic osteopathy show a correlation with body weight, markers of bone resorption and diabetic complications/co-morbidities (nephropathy, hypertension) being therefore not only an a priori consequence but also a complication of diabetes mellitus. Our data provide baseline data of QUS in type 1 diabetic patients. Because of the frequency of lower bone mineral content and their known high fracture risk bone metabolism screening of T1DM patients has to be considered.]
[Higher bone fracture prevalence in postmenopausal pollen allergic women]
[Our aim was to investigate whether pollen allergy can affect bone mass and fractures in postmenopausal women. A total of 125 postmenopausal pollen allergic women (mean age 61.26 years) were split into four groups: treated neither with H1 histamine receptor (H1R) antagonist nor with inhaled corticosteroid (n=43), treated only with H1R antagonist (n=53), treated both with H1R antagonist and inhaled corticosteroid (n=17), treated only with inhaled corticosteroid (n=12) for at least five years, seasonally. One-hundred non-allergic postmenopausal subjects matched for age, body mass index (BMI) and age at menopause served as controls. Overweight and obesity (25 kg/m2 ≤ BMI) were common among allergic women (76%). Allergic patients without treatment had a slightly lower bone density than their non-allergic mates. Untreated allergic had almost triple the rate of prevalent low-energy fractures (distal forearm, hip and clinical vertebral fractures: 34.9%) compared to non-allergic women (13%, χ2 p=0.003). Bone fracture occurred more often in H1R-only treated patients (30.19%) than in controls (χ2 p=0.01), however, clinical vertebral or hip fractures developed neither in those treated only with H1R antagonist nor in those who received both H1R antagonist and inhaled corticosteroid. Bone fractures were more frequent among patients with inhaled steroid treatment than among patients with a combined treatment of inhaled steroid and antihistamine (50% vs. 29.4%). BMI predicted prevalent fractures at 1.278 (95% CI, 1.047 to 1.559, p=0.016) for 1 kg/m2 increase among untreated allergic patients. In conclusion we found a high prevalence of low-energy fractures among pollen-allergic postmenopausal women, which was associated with obesity. It is possible that the H1R antagonists compensate for the negative effect of pollen-allergy and the adverse effect of inhaled corticosteroid treatment on bone fracture risk.]
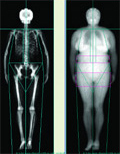
[The influence of menopause-related obesity and related changes of body fat distribution on the severity of sleep apnea]
[INTRODUCTION - The menopause is associated with an enhanced risk of obesity. During the postmenopausal period changes in the distribution of body fat lead to a variety of disorders. Obesity is among the major risk factors for Obstructive Sleep Apnea Syndrome (OSAS). The prevalence of OSAS increases after the menopause. This study was intended to explore the relationship between the severity of sleep apnea and the quantity, as well as the distribution of body fat in postmenopausal women with this condition. PATIENTS AND METHODS - Sixty-two postmenopausal women (aged 58.6±7.4 years) were studied. Patients suffering from OSAS - established by cardiorespiratory polygraphy - were enrolled. None of the subjects received hormone replacement therapy during the trial. Total and regional quantity of body fat was determined by dualenergy X-ray absorptiometry (DXA). The distribution of body fat, the ratio of android-to-gynoid regional fat, as well as body mass index were automatically calculated by the software of the DXA machine. A specific region was defined to measure the fat content of the cervical region, extending from the mental protuberance to the clavicular plane. The reliability coefficient of the test method was calculated to check the accuracy of regional body fat measurement. The severity of obstructive sleep apnea was determined by cardiorespiratory polygraphy and expressed using the apnea/hypopnea index. RESULTS - Testing for independence in this population revealed the lack of independence between android-type obesity and severe OSAS. Specifically, 74% of patients with severe OSAS were obese (BMI>30 kg/m2). As with the android-type, the khi square test similarly refuted the independence between obesity and the severity of OSAS. Fat content of the cervical region was 25.2% in mild and moderate, and 30.2% in severe OSAS. Two-Sample t-test demonstrated the significant influence of cervical fat content on OSAS severity. CONCLUSION - Elevated BMI, android-type obesity, and higher relative fat content of the cervical region all aggravate obstructive sleep apnea in postmenopausal women.]
[The rehabilitation team and distinct representatives of medicine in the service of osteopenic patients]
[The rehabilitation team and distinct representatives of medicine in the service of osteopenic patients 2007;10(01)]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
3.
4.
5.